This document discusses various disorders of the tongue and taste, including:
- Developmental tongue disorders like microglossia and macroglossia. Lingual thyroid is also discussed.
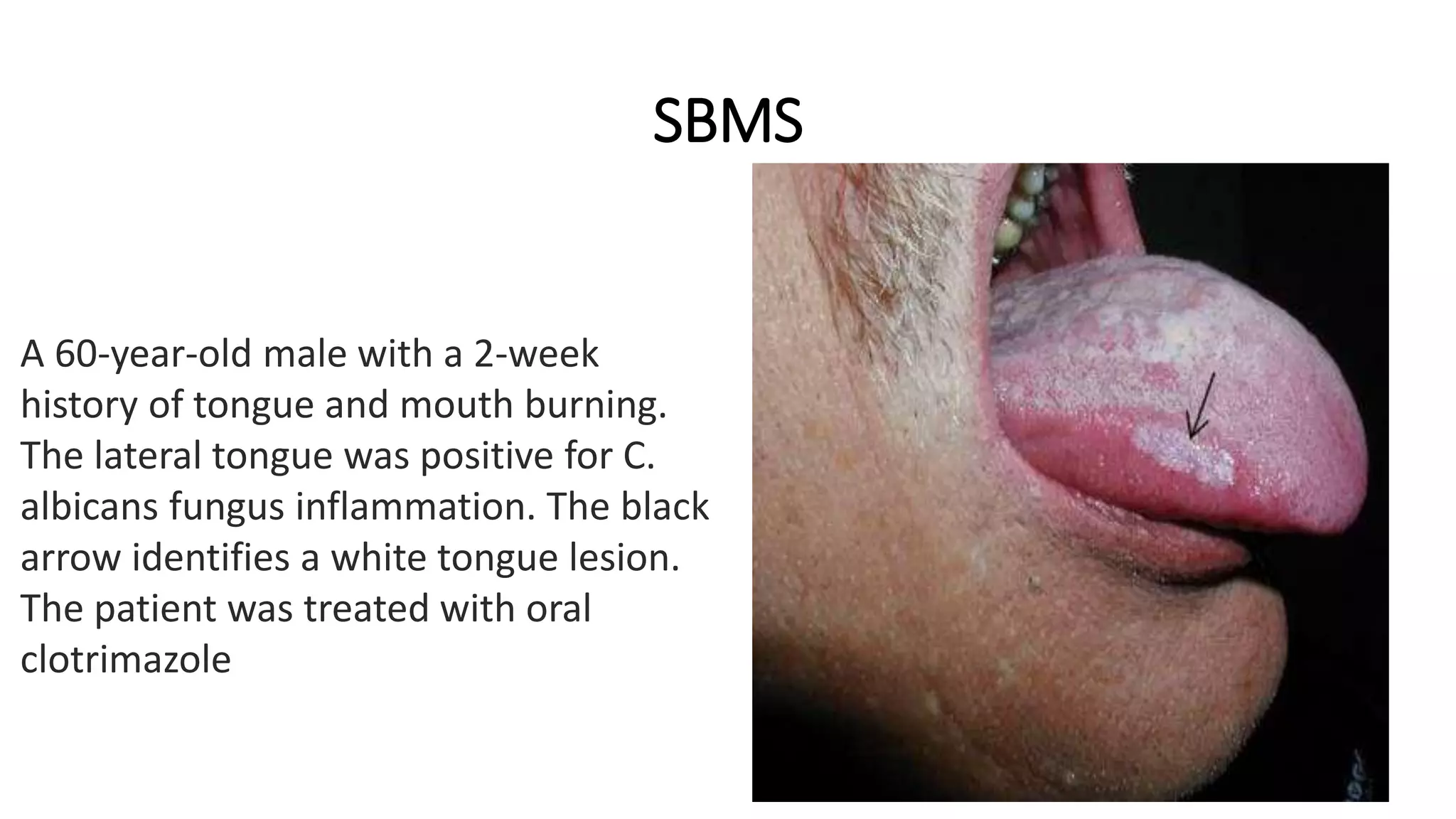
- Infections of the tongue caused by viruses like HSV and fungi like Candida. EBV can cause oral hairy leukoplakia.
- HIV/AIDS can be associated with oral candidiasis, histoplasmosis, and oral hairy leukoplakia of the tongue.
- Taste abnormalities like ageusia, hypogeusia, hypergeusia and dysgeusia are also summarized.




































![G)KAPOSI’S SARCOMA
• Multifocal neoplasm of vascular endothelial cell origin.
• About 15% to 20% of patients with AIDS demonstrate KS.
• Human herpesvirus type 8 (HHV-8, Kaposi’s sarcoma– associated herpesvirus[KSHV]) is noted
within the tumor and believed to be responsible for the neoplasm’s development.
• KS typically manifests as multiple lesions of the skin or oral mucosa.
• The trunk, arms, head, and neck are the most commonly involved anatomic sites (Fig. 7-38).
• Approximately 70% of individuals with HIV-related KS of skin or viscera demonstrate oral lesions; in
22% the oral cavity is the initial site of involvement.
• Although any mucosal site may be involved, the hard palate, gingiva, and tongue are affected most
frequently .
• The lesions begin as brown or reddish purple macular lesions that do not blanch with pressure.
• With time, the macules typically develop into plaques or nodules .
• Pain, bleeding, and necrosis may become a problem and necessitate therapy](https://image.slidesharecdn.com/tonguetastedisorders-230509235555-bb0a9bb9/75/TONGUE-TASTE_DISORDERS-pptx-39-2048.jpg)