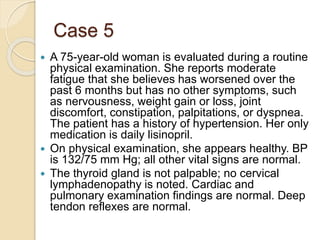
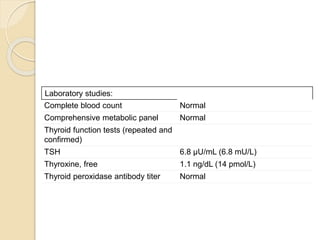
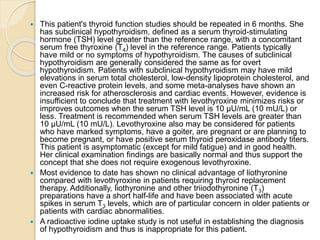
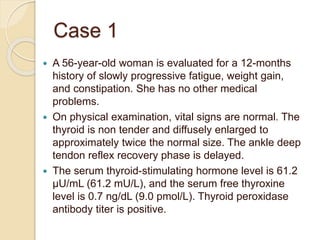
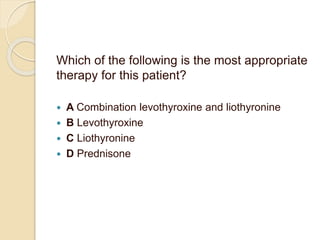
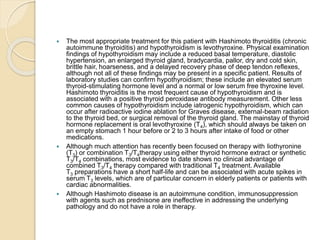
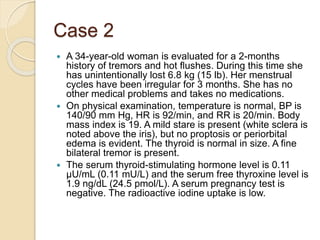
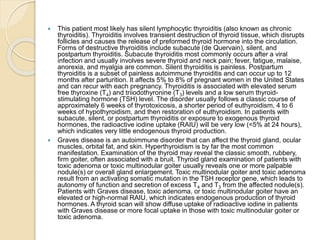
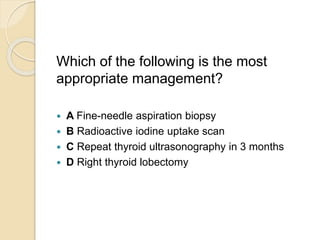
This document discusses 6 cases involving thyroid disorders. Case 1 involves a 56-year-old woman with fatigue, weight gain, and constipation diagnosed with Hashimoto's thyroiditis and hypothyroidism. Case 2 involves a 34-year-old woman with tremors, hot flushes, and weight loss diagnosed with silent lymphocytic thyroiditis. Case 3 involves a 40-year-old man with a thyroid nodule found on exam who should undergo fine-needle aspiration biopsy. Case 4 involves management of levothyroxine dosage for a pregnant woman with hypothyroidism. Case 5 involves a 75-year-old woman with fatigue and subclinical hypothyroidism who should repeat thyroid testing


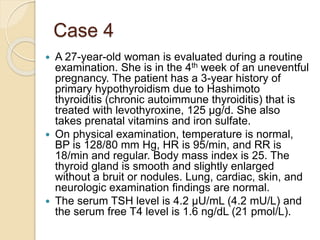
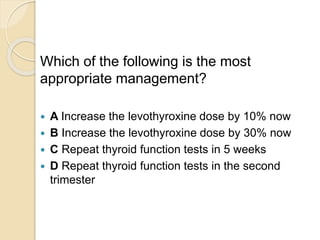
![ This patient's levothyroxine (T4) dose should be increased by 30%
now, and the thyroid function tests should be repeated in 2 to 4 weeks.
Pregnancy is known to increase levothyroxine requirements in most
patients receiving thyroid replacement therapy, and this expected
increase should be anticipated by increasing the levothyroxine dose.
This is typically increased in the first (and sometimes in the second)
trimester of pregnancy, with a possible total increase of 30% to 50%,
and an increase in levothyroxine dose in this range to maintain the
thyroid-stimulating hormone (TSH) level between approximately 0.1
and 2.5 µU/mL (0.1-2.5 mU/L) is associated with fewer maternal and
fetal complications. The fetus is largely dependent on transplacental
transfer of maternal thyroid hormones during the first 12 weeks of
gestation, and the presence of maternal subclinical or overt
hypothyroidism may be associated with subsequent fetal
neurocognitive impairment, increased risk of premature birth, low birth
weight, increased miscarriage rate, and even an increased risk of fetal
death. In pregnant women with hypothyroidism, thyroid function testing
should be frequent, preferably every 4 weeks, to protect the health of
mother and fetus and to avoid pregnancy complications.
Continuing the current levothyroxine dose is inappropriate in this
patient because her TSH level is already too high (4.2 µU/mL [4.2
mU/L]). TSH levels generally should range from 0.1 to 2.5 µU/mL (0.1-
2.5 mU/L) in the first trimester, 0.2 to 3.0 µU/mL (0.2-3.0 mU/L) in the
second trimester, and 0.3 to 3.0 µU/mL (0.3-3.0 mU/L) in the third
trimester.](https://image.slidesharecdn.com/thyroiddisordersmed3lecture-211210203357/85/Thyroid-disorders-13-320.jpg)