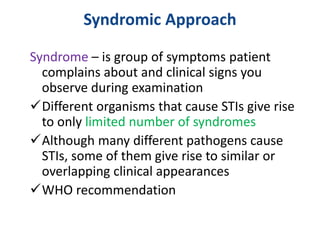
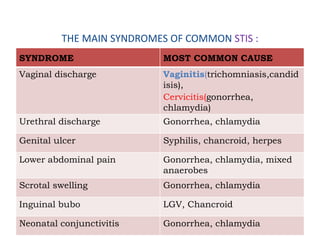
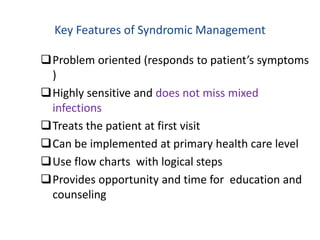
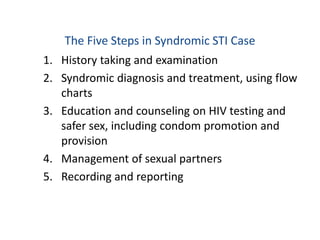
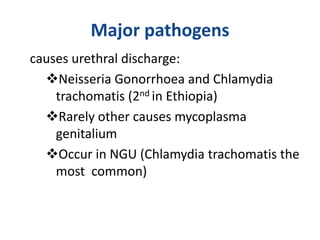
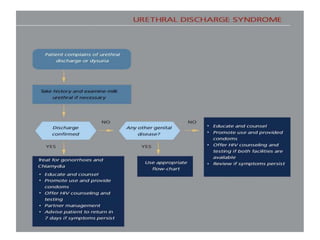
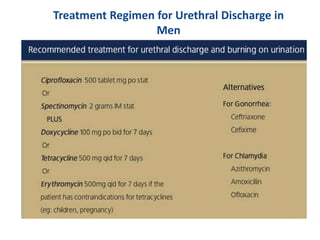
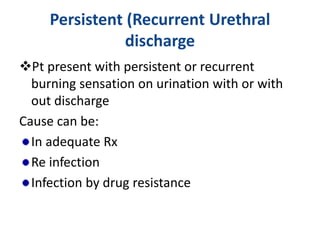
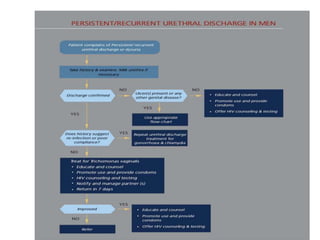
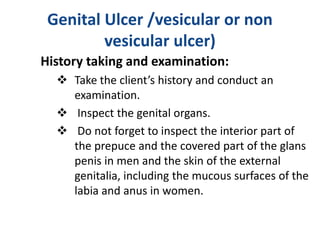
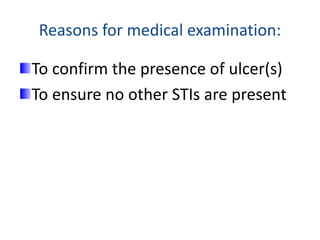
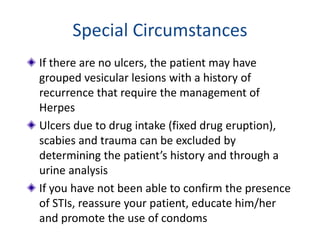
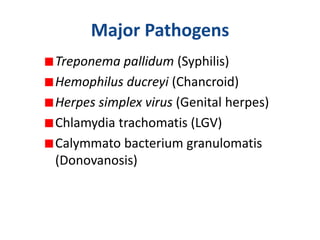
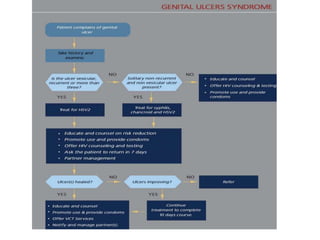
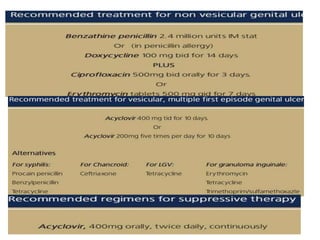
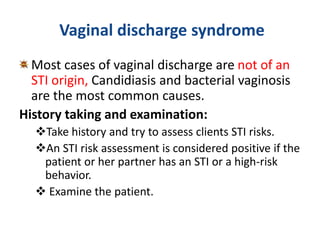
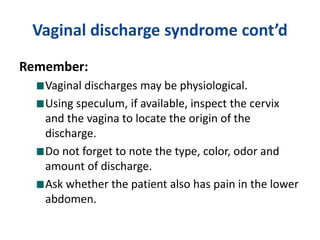
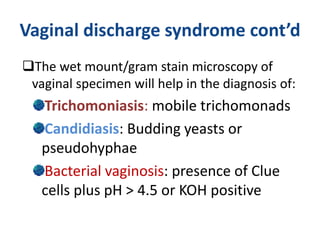
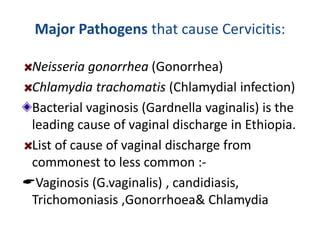
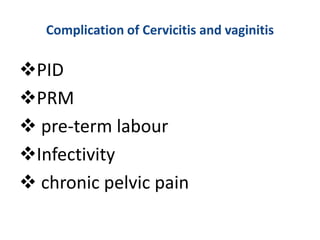
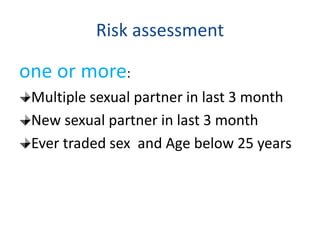
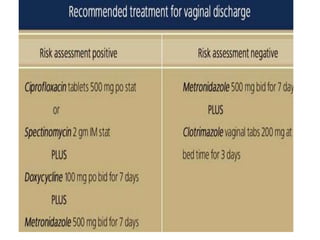
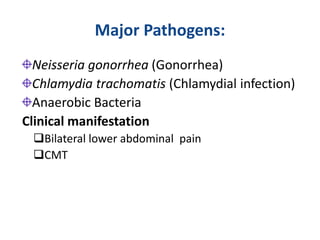
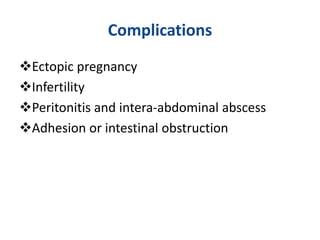
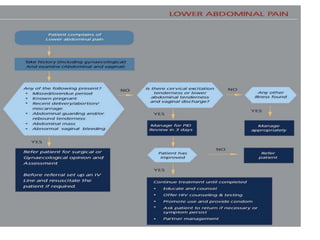
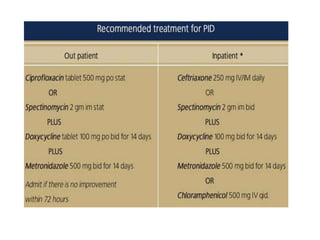
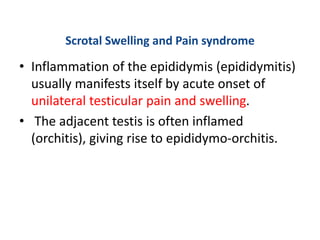
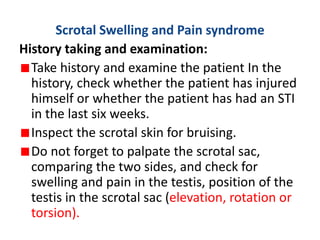
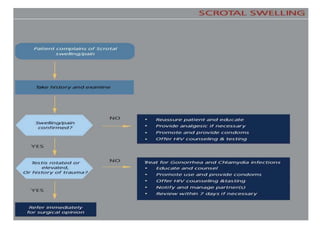
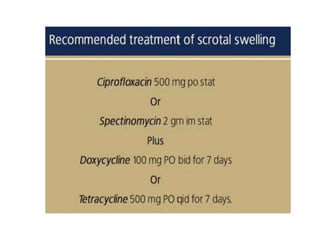
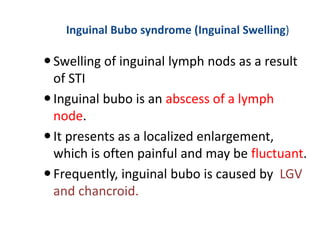
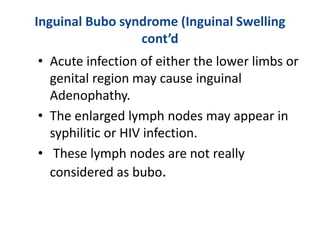
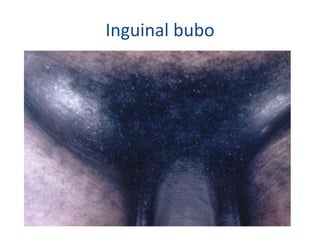
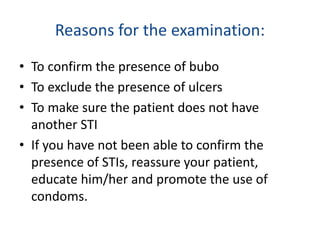
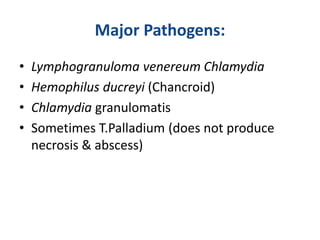
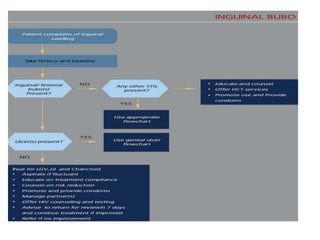
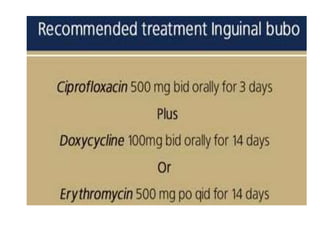
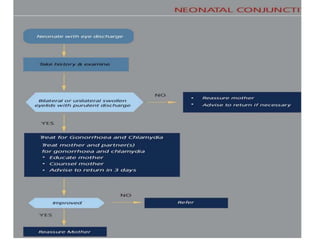
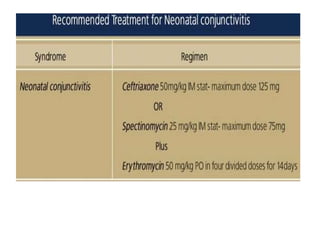
This document discusses the syndromic approach to diagnosing and treating sexually transmitted infections (STIs). It describes how STIs present as distinct syndromes based on their symptoms and signs. Using flowcharts, healthcare workers can diagnose and treat patients based on their presenting syndrome rather than attempting to identify the specific pathogen. This approach is recommended by the WHO as it is more accurate than clinical judgment alone and allows for treatment at the first visit. The document then outlines the main STI syndromes and their typical causes.