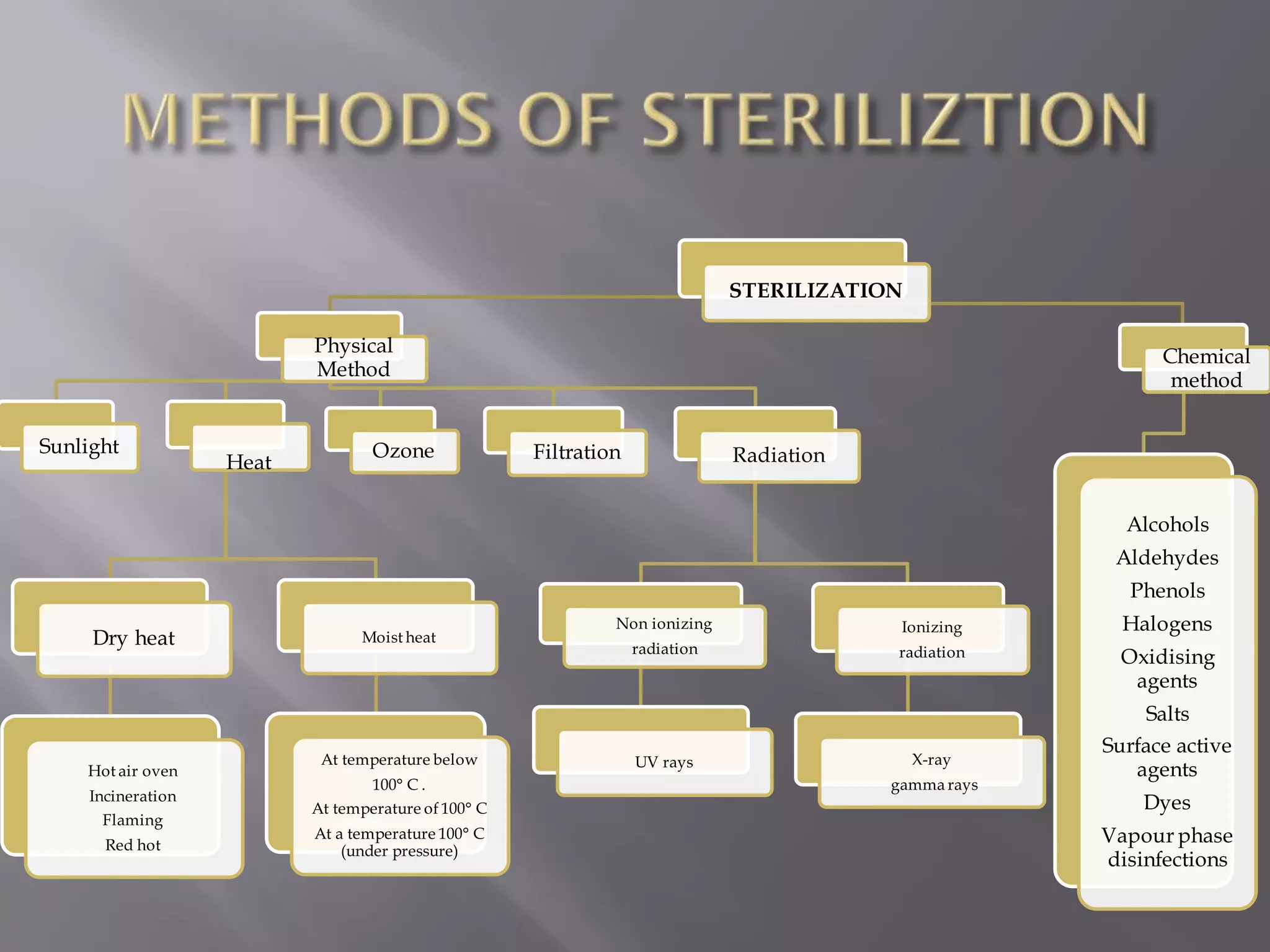
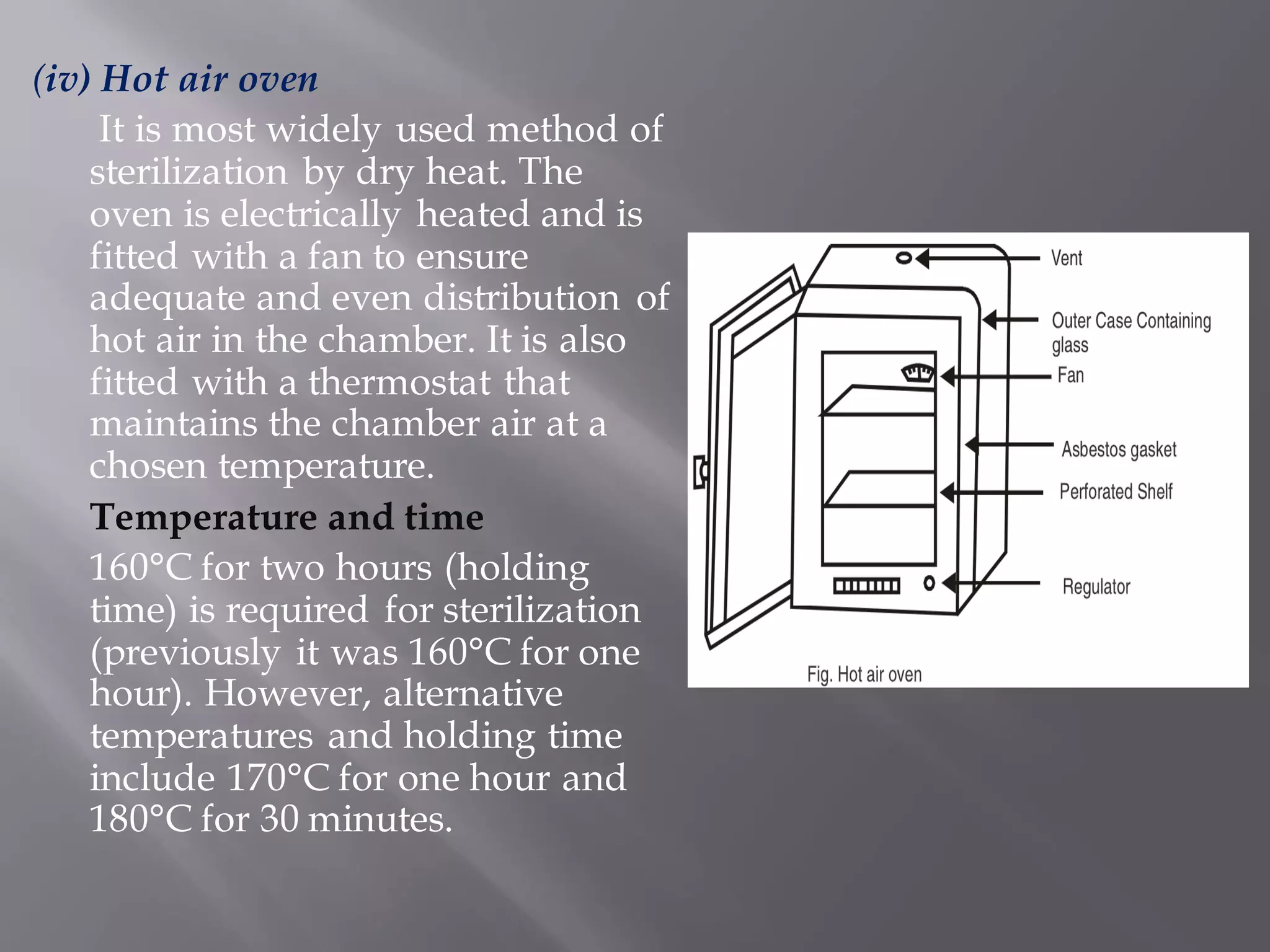
This document discusses various sterilization methods used in hospitals including physical, chemical, and radiation-based methods. Physical sterilization methods include heat sterilization using dry heat like hot air ovens or moist heat like autoclaves. Chemical sterilization uses disinfecting agents like alcohols, aldehydes, and phenols. Radiation sterilization employs ionizing radiation from X-rays or gamma rays and non-ionizing radiation like UV rays. Proper sterilization is essential for destroying microorganisms on medical equipment and surfaces to prevent contamination and infection in hospitals.