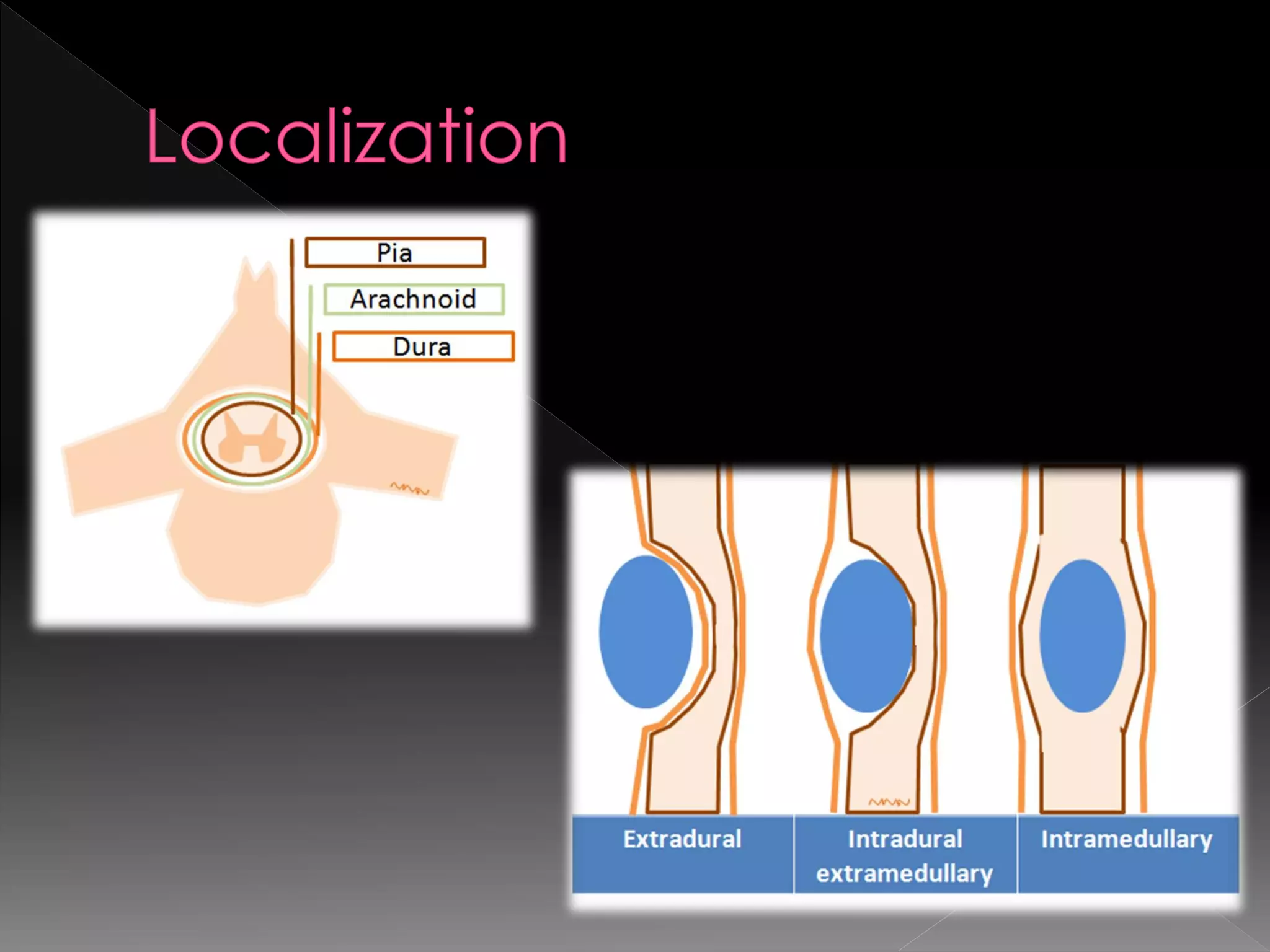
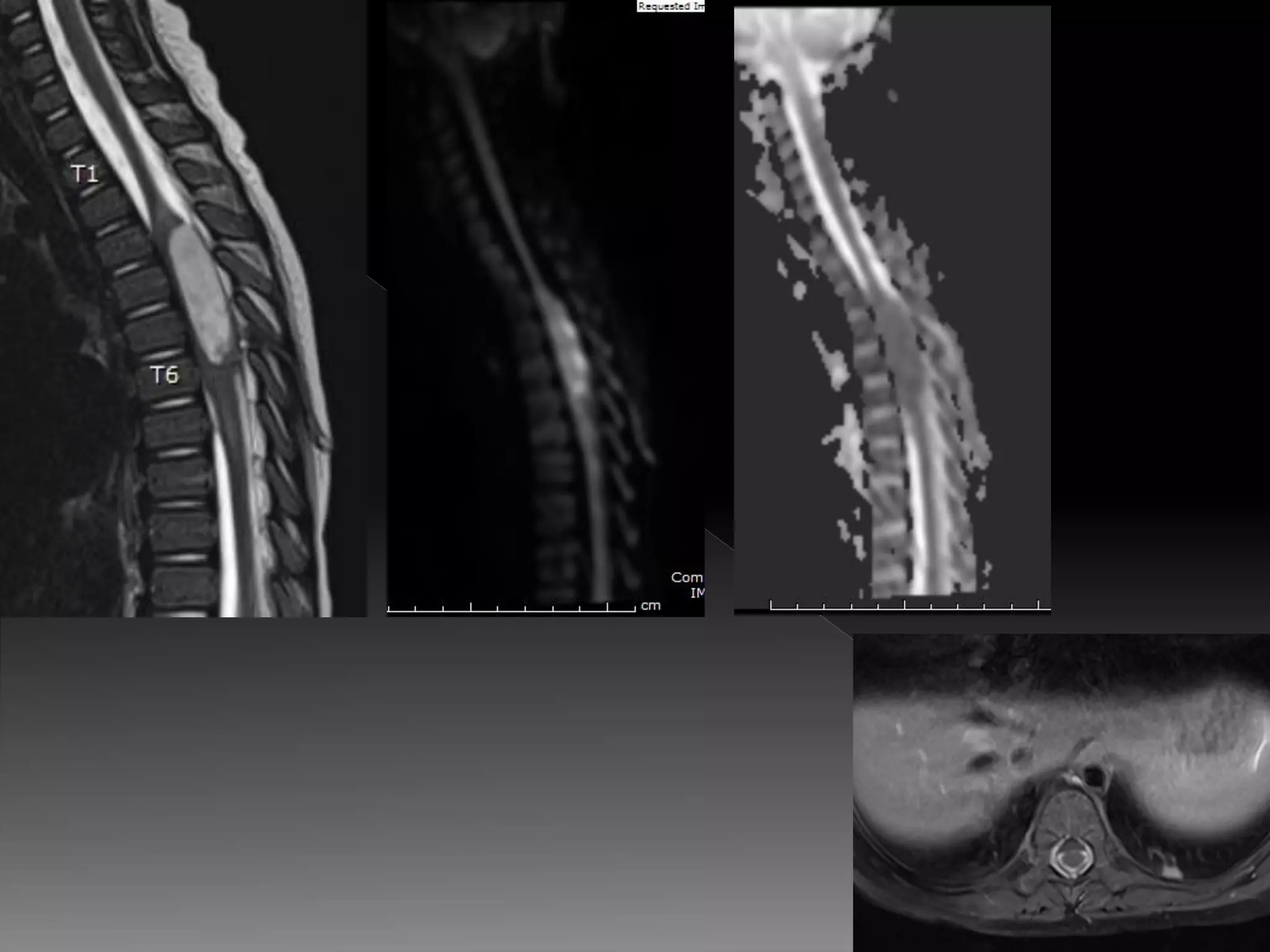
This document discusses the localization, characterization, and key imaging features of various spinal tumors. It covers both intradural and extradural tumors, including their location within or outside the spinal cord. Common tumor types discussed include ependymoma, astrocytoma, hemangioblastoma, and spinal cord metastases. Key distinguishing imaging features between tumor types are provided, such as differences in location, enhancement patterns, presence of cysts, and association with other findings.