The Sphere Project was initiated to improve humanitarian response quality and accountability. It established minimum standards in key sectors based on the rights of disaster-affected populations to life with dignity and assistance. The Sphere Handbook contains the Humanitarian Charter and minimum standards in water, sanitation, food, shelter, and health. It provides guidance for principled and effective humanitarian action that meets universally agreed-upon quality and accountability standards.





































































































































































































































































































































































































![+XPDQLWDULDQKDUWHUDQG0LQLPXP
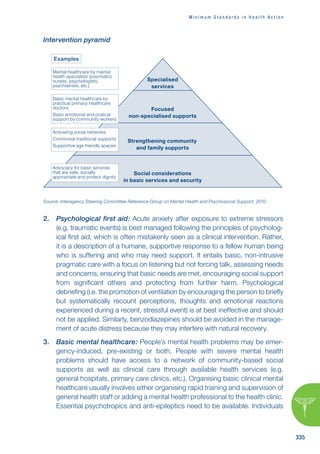
6WDQGDUGVLQ+XPDQLWDULDQ5HVSRQVH
7KHULJKWWROLIHZLWKGLJQLW
;OL:WOLYL7YVQLJ[PZHUPUP[PH[P]L[VKL[LYTPULHUK
WYVTV[LZ[HUKHYKZI`^OPJO[OLNSVIHSJVTTUP[`
YLZWVUKZ[V[OLWSPNO[VMWLVWSLHMMLJ[LKI`KPZHZ[LYZ
P[O[OPZ/HUKIVVR:WOLYLPZ^VYRPUNMVYH^VYSKPU^OPJO
[OLYPNO[VMHSSWLVWSLHMMLJ[LKI`KPZHZ[LYZ[VYLLZ[HISPZO[OLPY
SP]LZHUKSP]LSPOVVKZPZYLJVNUPZLKHUKHJ[LKWVUPU^H`Z[OH[
YLZWLJ[[OLPY]VPJLHUKWYVTV[L[OLPYKPNUP[`HUKZLJYP[`
This Handbook contains:
(/THUP[HYPHU*OHY[LY!SLNHSHUKTVYHSWYPUJPWSLZ^OPJO
YLÅLJ[[OLYPNO[ZVMKPZHZ[LYHMMLJ[LKWVWSH[PVUZ
7YV[LJ[PVU7YPUJPWSLZ
*VYL:[HUKHYKZHUKTPUPTTZ[HUKHYKZPUMVYRL`SPMLZH]PUN
OTHUP[HYPHUZLJ[VYZ!H[LYZWWS`ZHUP[H[PVUHUKO`NPLUL
WYVTV[PVU-VVKZLJYP[`HUKU[YP[PVU:OLS[LYZL[[SLTLU[HUK
UVUMVVKP[LTZ/LHS[OHJ[PVU;OL`KLZJYPILwhat needs to be
achieved in a humanitarian response in order for disaster-
affected populations to survive and recover in stable
conditions and with dignity.
;OL:WOLYL/HUKIVVRLUQV`ZIYVHKV^ULYZOPWI`HNLUJPLZHUK
PUKP]PKHSZVMMLYPUN[OLOTHUP[HYPHUZLJ[VYH common language
for working together towards quality and accountability in
disaster and conflict situations
;OL:WOLYL/HUKIVVROHZHUTILYVMºJVTWHUPVU
Z[HUKHYKZ»L_[LUKPUNP[ZZJVWLPUYLZWVUZL[VULLKZ[OH[
OH]LLTLYNLK^P[OPU[OLOTHUP[HYPHUZLJ[VY
;OL:WOLYL7YVQLJ[^HZPUP[PH[LKPU I`HUTILY
VMOTHUP[HYPHU5.6ZHUK[OL9LK*YVZZHUK
9LK*YLZJLU[4V]LTLU[](https://image.slidesharecdn.com/sphereproject-221012110215-04299518/85/sphere-project-pdf-402-320.jpg)