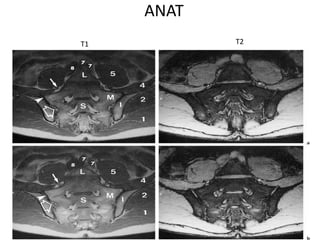
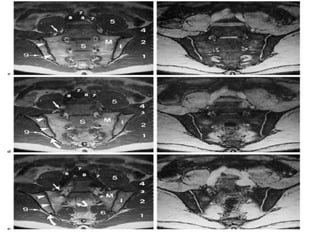
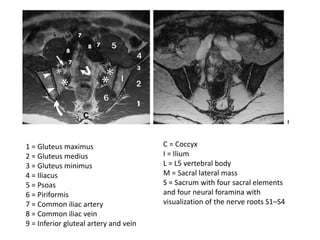
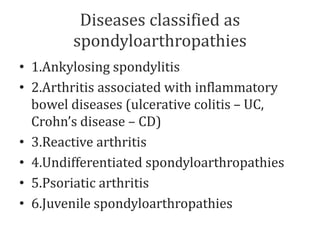
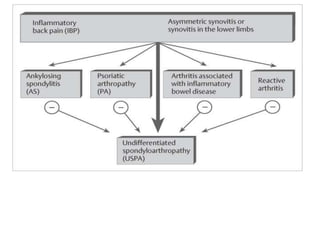
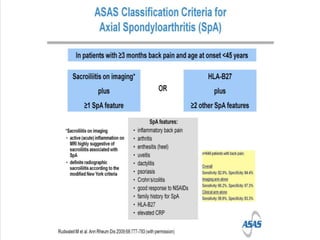
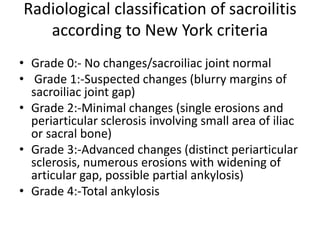
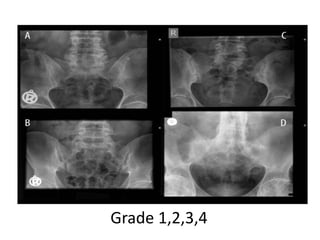
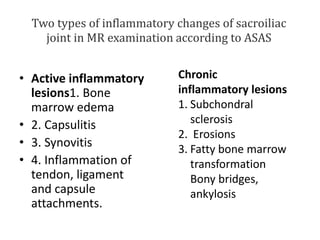
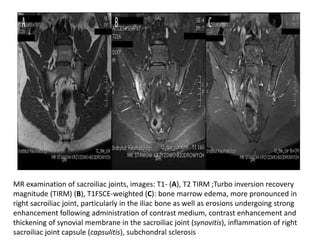
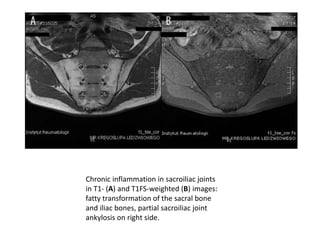
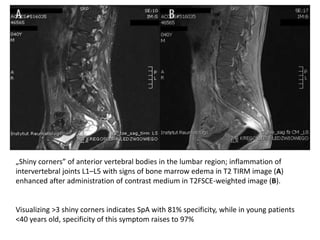
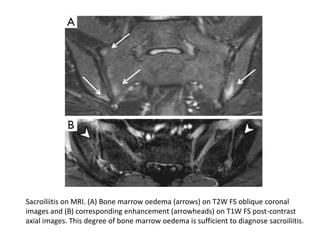
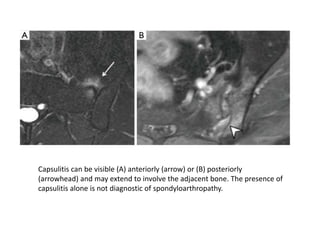
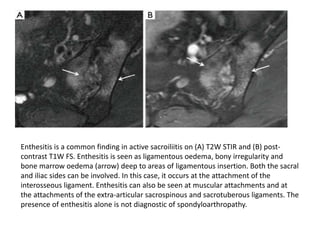
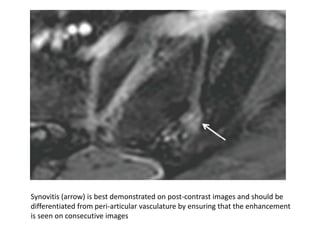
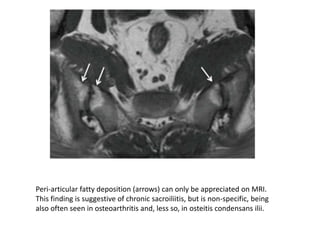
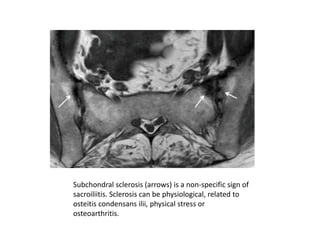
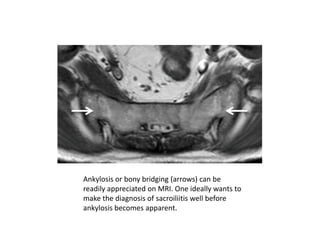
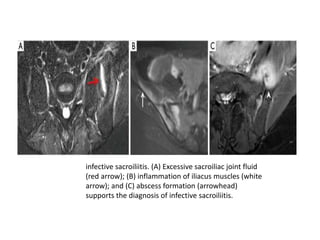
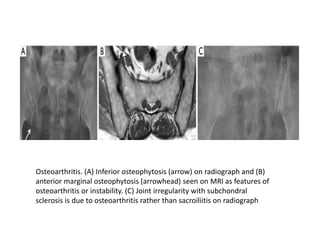
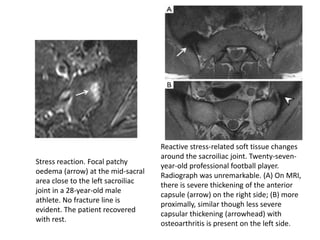
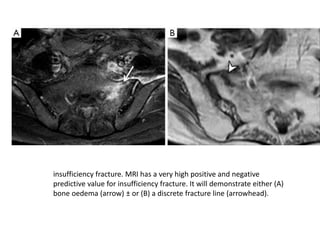
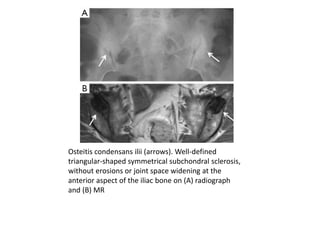
This document summarizes pathologies of the sacroiliac (SI) joint that can be identified on MRI. It describes the anatomy of the SI joint and classifies diseases as spondyloarthropathies. Signs of active inflammation on MRI include bone marrow edema, synovitis, capsulitis, and enthesitis. Chronic changes include subchondral sclerosis, erosions, and ankylosis. Differential diagnoses discussed are infective sacroiliitis, osteoarthritis, stress reactions, insufficiency fractures, and osteitis condensans ilii. Images are provided to illustrate the radiological findings of various SI joint pathologies.