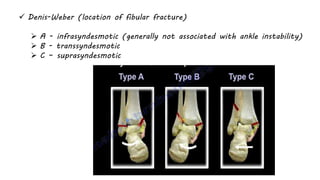
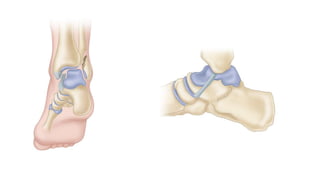
This document provides an overview of ankle fracture patterns, classifications, radiographic evaluation, treatment approaches, and postoperative management. Key points include that ankle fractures can be classified anatomically or using the Lauge-Hansen system, radiographs include stress views to assess ligament injuries, treatment depends on fracture displacement and stability, and goals are anatomic reduction and fixation to restore the ankle mortise. Complications include wound issues, infection, and post-traumatic arthritis.