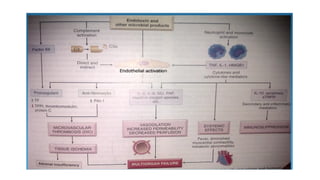
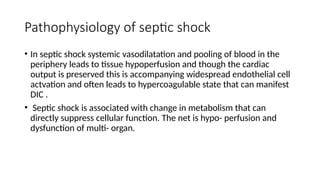
The document outlines the clinical syndrome of shock, characterized by inadequate tissue perfusion leading to cellular death and potential organ failure. It classifies shock into various types, including hypovolemic, cardiogenic, septic, traumatic, neurogenic, and hypoadrenal shock, detailing their etiology, pathogenesis, clinical presentation, and morphological changes in affected organs. Additionally, it discusses the stages of shock and their complications, emphasizing the physiological mechanisms and effects on multiple organ systems.