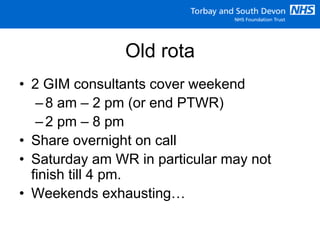
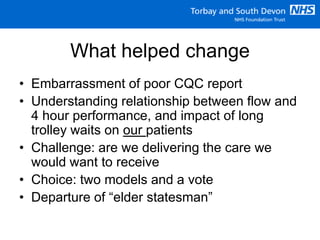
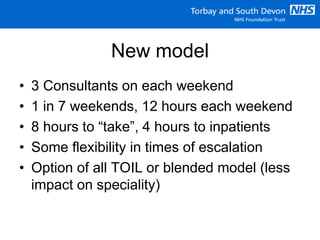
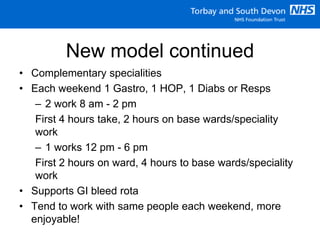
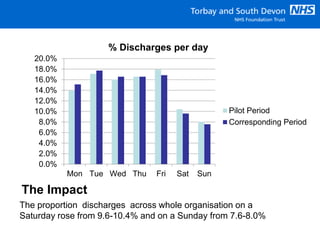
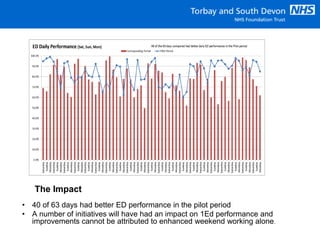
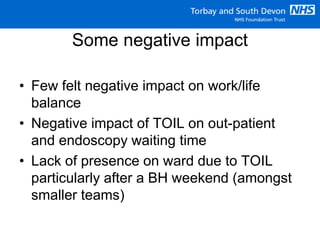
The document discusses the implementation of a new weekend ward round model at Torbay and South Devon NHS Foundation Trust aimed at improving consultant availability and patient flow. The new model, which includes three consultants each weekend and revised scheduling, resulted in improved patient outcomes and greater satisfaction among staff. Pilot data showed an increase in discharges on weekends and improved overall performance metrics, although some negative impacts on outpatient services were noted.