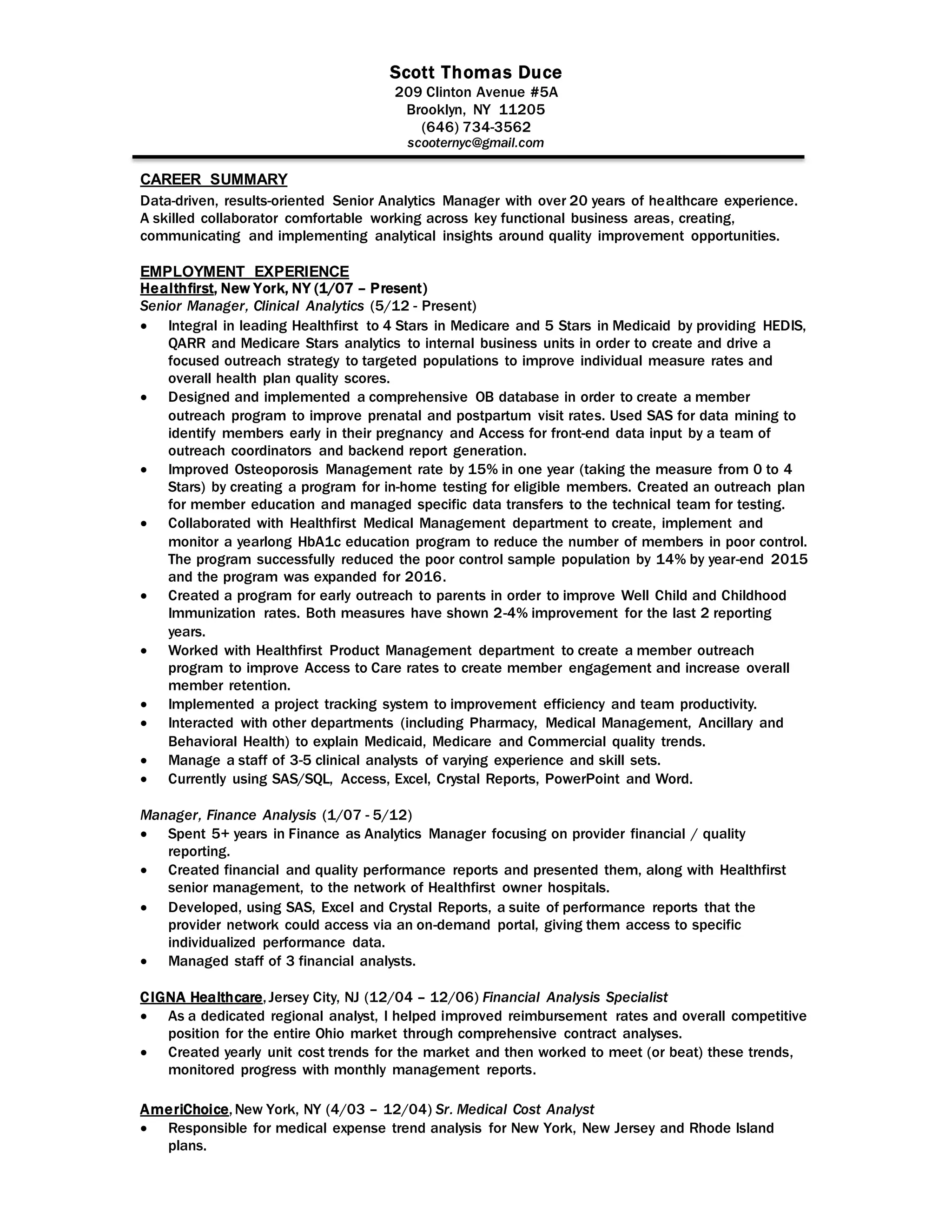
Scott Thomas Duce has over 20 years of experience in healthcare analytics and quality improvement. He currently works as a Senior Manager of Clinical Analytics at Healthfirst, where he has led initiatives to improve star ratings and health outcomes. These initiatives include creating programs for prenatal visits, osteoporosis testing, diabetes education, well-child visits, and access to care. He also manages a team of clinical analysts and has experience in finance analytics.