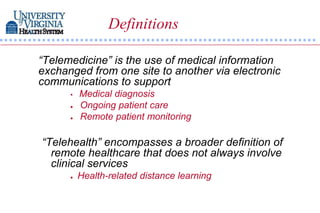
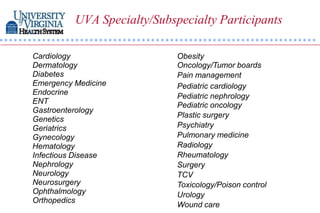
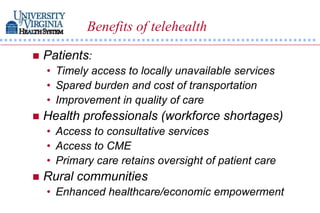
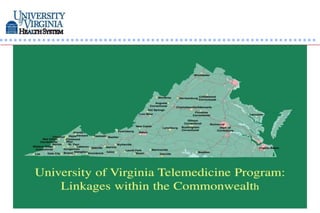
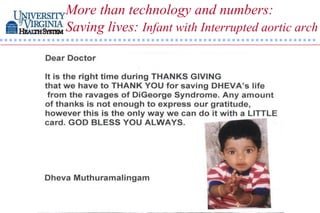
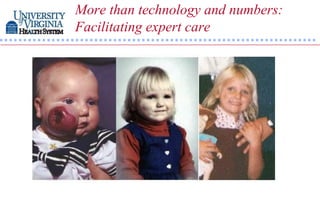
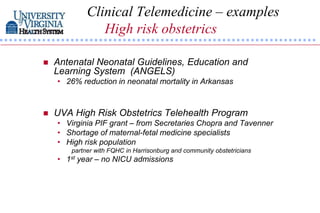
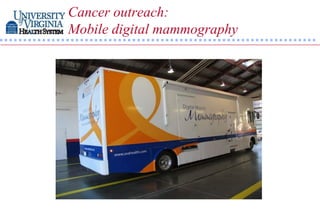
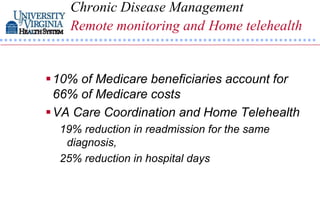
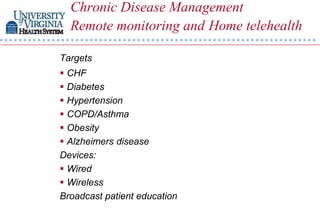
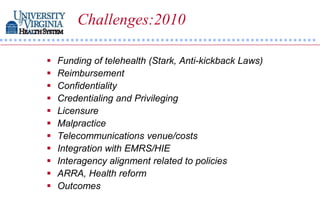
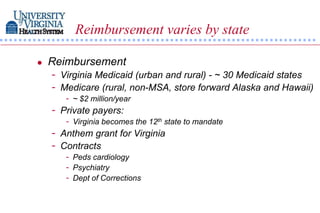
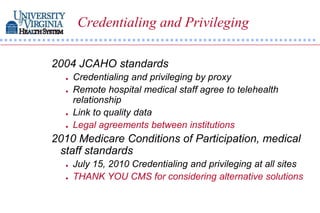
This document discusses telehealth and its use as a tool for healthcare in the 21st century. It defines telehealth and telemedicine, and describes how the University of Virginia uses telehealth for clinical care, teaching, research, and public service in over 30 specialties. Telehealth benefits patients through improved access to care, health systems through workforce support, and rural communities through enhanced healthcare. The document outlines federal and state support for telehealth and examples of clinical telehealth programs, including high risk obstetrics, tele-ophthalmology, pediatric cardiology, stroke care, cancer, tele-pathology, and chronic disease management. Challenges to telehealth include funding, reimbursement, licensure and others.