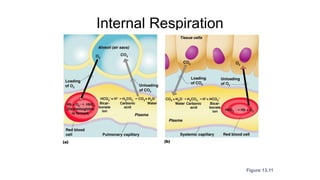
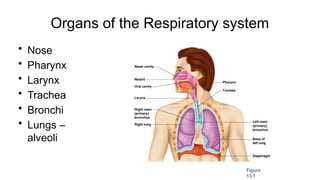
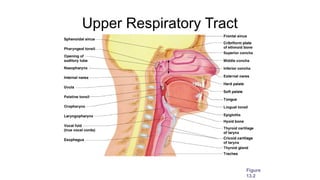
The document outlines the anatomy and function of the respiratory system, detailing the organs involved in gas exchange, including the nose, pharynx, larynx, trachea, bronchi, and lungs. It describes the mechanics of breathing, pulmonary ventilation, and the processes of external and internal respiration, as well as factors influencing respiratory rates. Additionally, it covers respiratory disorders, developmental aspects, and aging effects on the respiratory system.
![Gas Transport in the Blood
• Oxygen transport in the blood
– Inside red blood cells attached to hemoglobin
(oxyhemoglobin [HbO2])
– A small amount is carried dissolved in the
plasma
• Carbon dioxide transport in the blood
– Most is transported in the plasma as
bicarbonate ion (HCO3–)
– A small amount is carried inside red blood
cells on hemoglobin, but at different binding
sites than those of oxygen](https://image.slidesharecdn.com/respiratorysystem-241111002317-e5c2ab01/85/Respiratory-System-pptxiiooooiikkjjjbbbb-39-320.jpg)