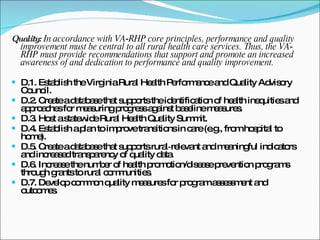
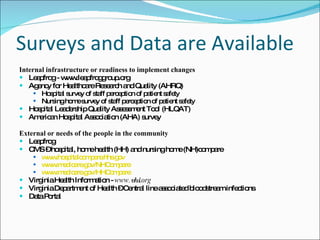
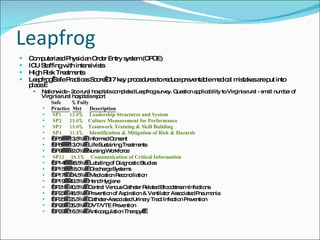
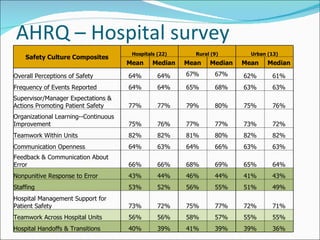
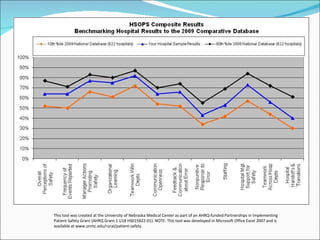
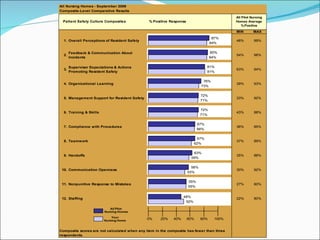
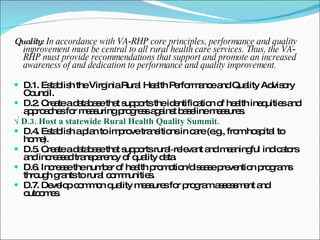
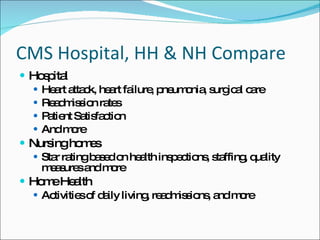
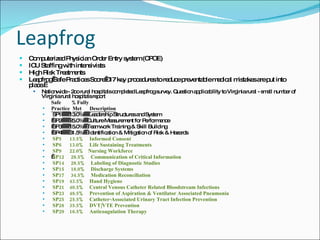
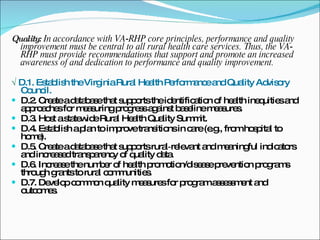
The document discusses quality improvement in rural healthcare settings in Virginia. It recommends establishing a Rural Health Performance and Quality Advisory Council to support quality improvement efforts. Several databases and quality measures are mentioned that could help measure progress, identify health inequities, and increase transparency of quality data. The document also discusses survey results showing areas for improvement in rural hospitals, such as staffing, handoffs, and nonpunitive responses to errors. It proposes expanding membership of the Advisory Council to include more stakeholders and continue planning quality improvement initiatives.