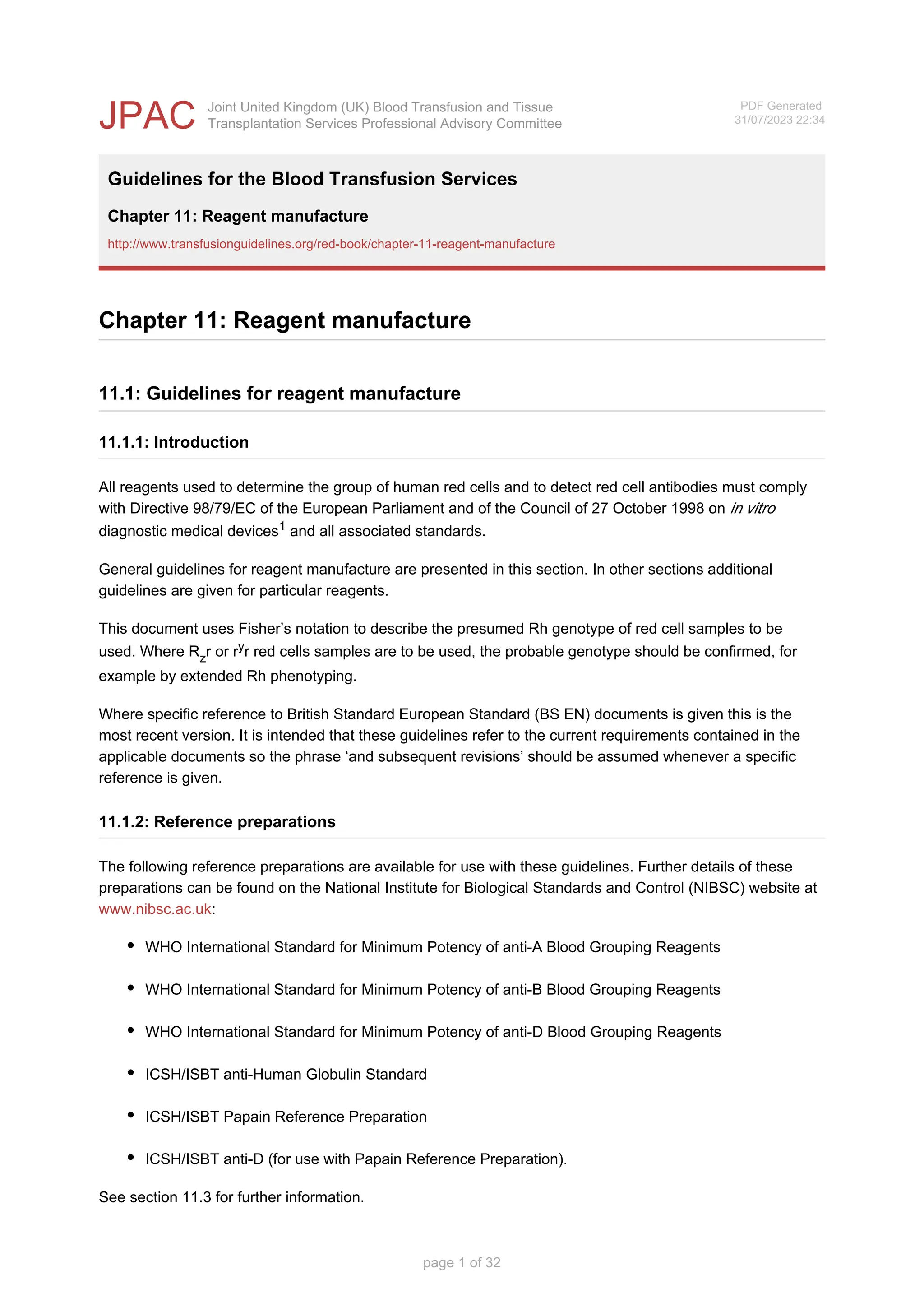
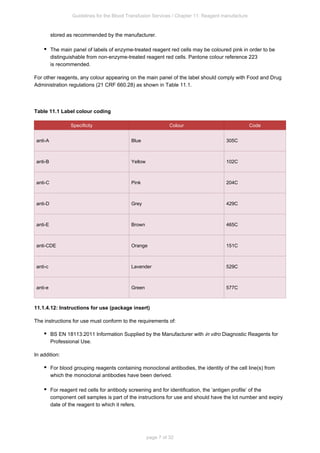
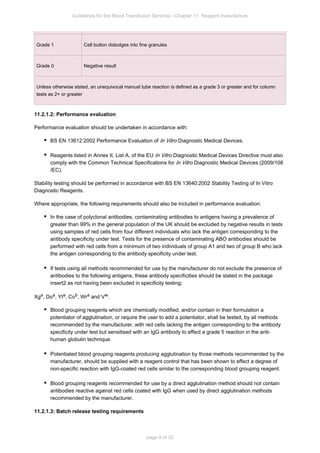
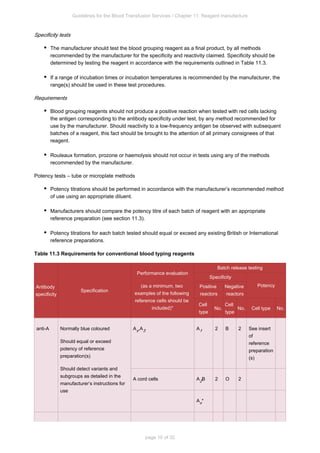
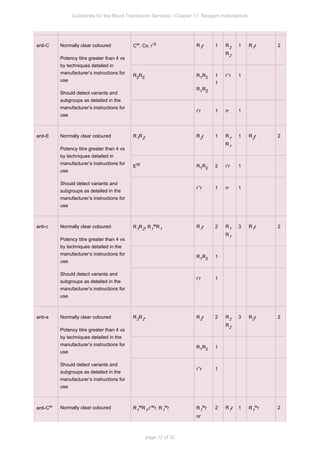
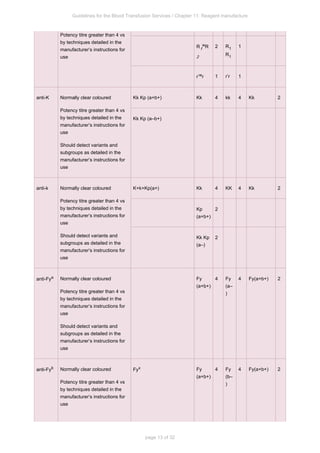
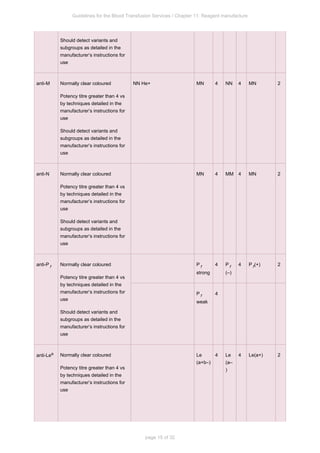
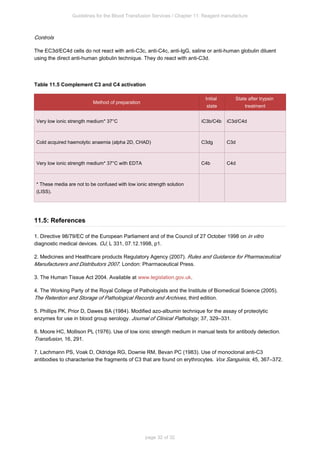
This document provides guidelines for the manufacture of reagents used for blood group serology. It discusses good manufacturing practices, reference preparations, definitions, general manufacturing considerations including risk management, performance evaluation, stability testing, and labeling requirements. Reagents must be manufactured according to applicable European directives and standards to ensure quality and safety.