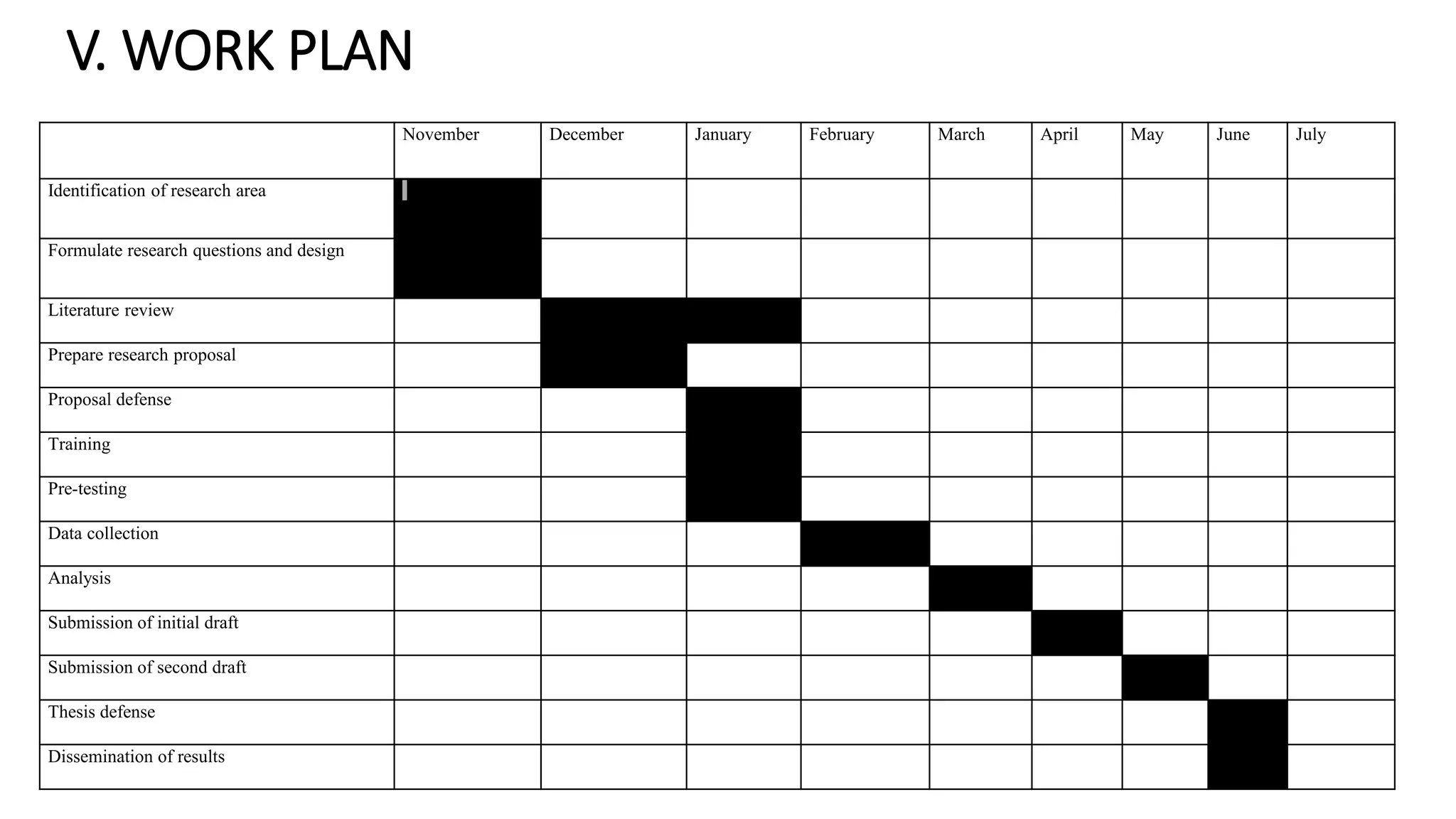
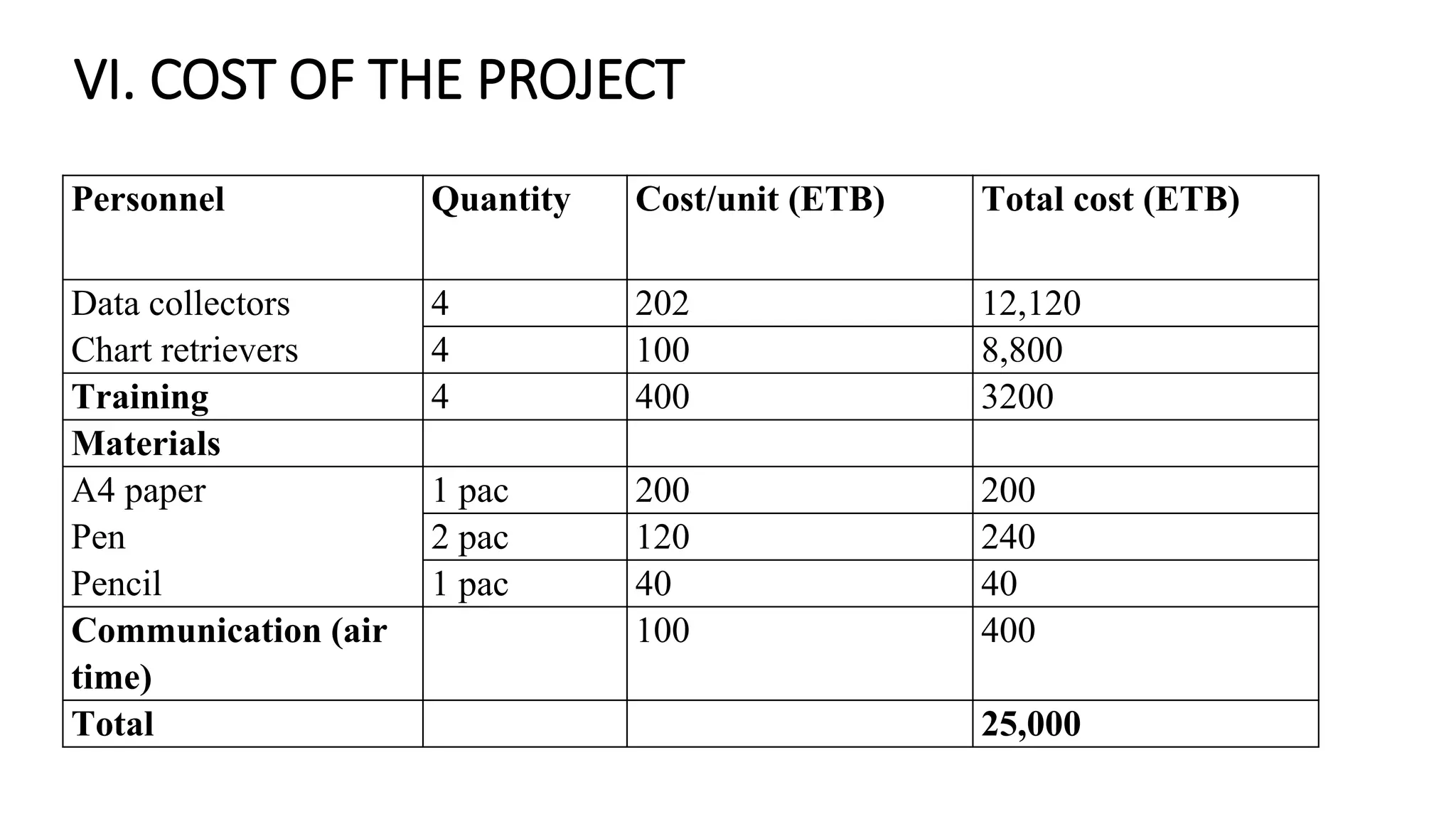
This proposal outlines a study on the experience of laparoscopic cholecystectomy (gallbladder removal surgery) at St. Paul's Hospital Millennium Medical College in Addis Ababa, Ethiopia. The study will retrospectively review medical records from 2015-2020 to evaluate postoperative complications, conversion rates from laparoscopic to open surgery, and factors associated with complications. The objectives are to assess complication patterns, determine factors linked to complications, and calculate conversion rates and reasons. The proposal describes the background, literature review, methods, work plan, and budget for the study.