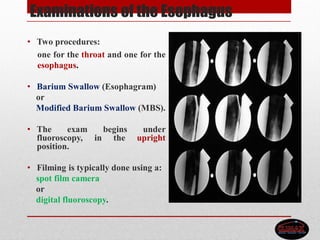
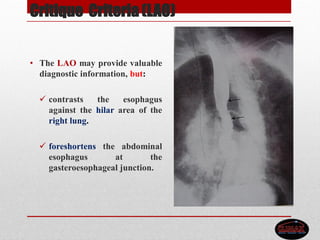
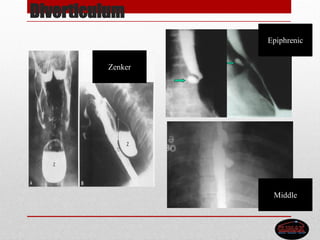
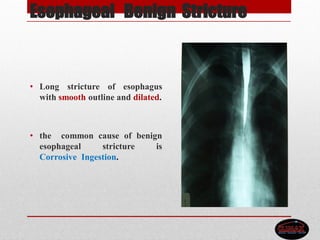
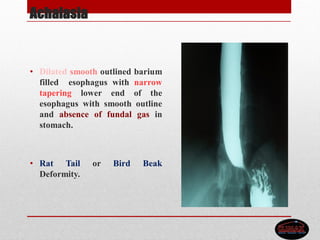
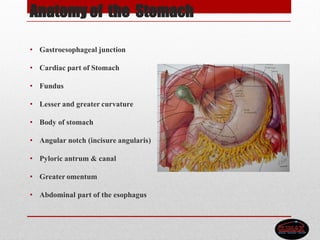
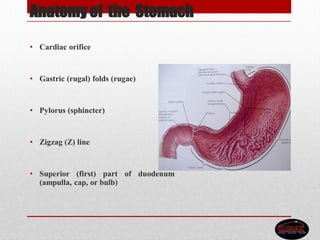
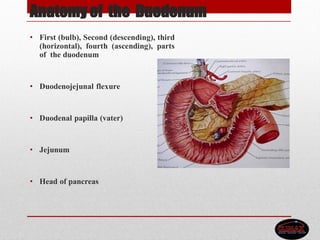
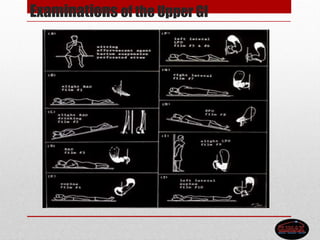
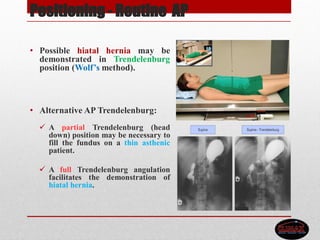
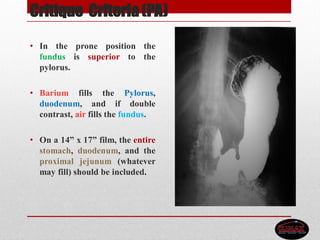
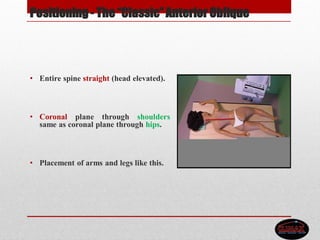
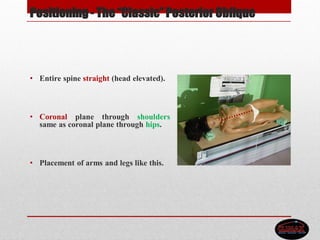
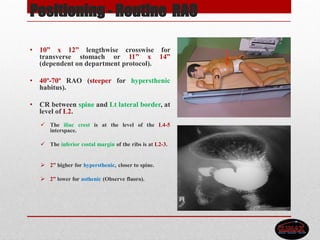
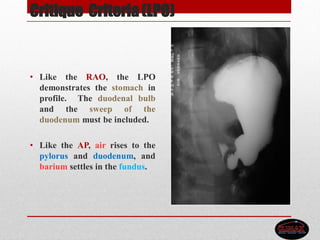
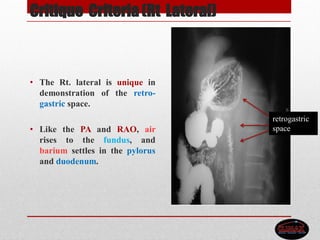
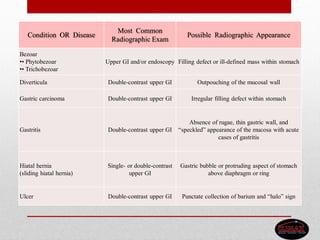
The document presents a comprehensive overview of barium swallow and meal procedures, detailing anatomical structures, examination techniques, patient preparation, and significant pathologies of the esophagus and stomach. It emphasizes the use of barium sulfate as a contrast medium, outlines various positioning techniques for imaging, and describes critique criteria for evaluating film quality. Additional sections cover the importance of proper patient preparation and highlight potential pathologies with their radiographic appearances.