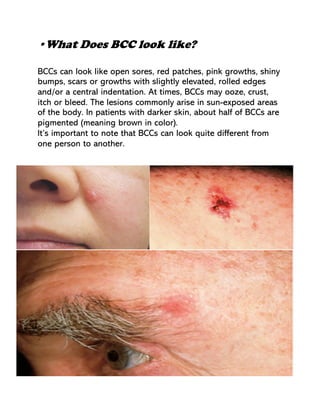
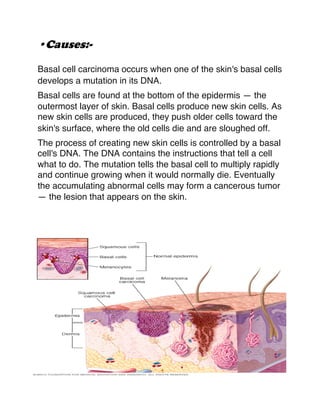
Basal cell carcinoma is the most common type of skin cancer. It occurs as a result of damage to skin cells called basal cells, usually due to sun exposure. Basal cell carcinoma appears as patches, open sores, bumps, or scars on sun-exposed areas like the head and neck. Risk factors include fair skin, sun exposure, age, and certain genetic conditions. Prevention focuses on limiting sun exposure and wearing protective clothing and sunscreen. Treatment options depend on the size and location of the cancer, and may include surgery, freezing, or creams.