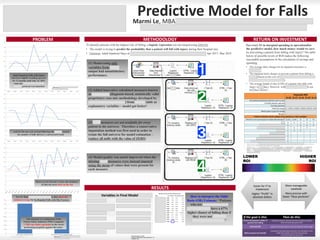
The document discusses a predictive model developed to identify adults at high risk of falling with injury during hospital stays, using various patient characteristics and risk factors. Following the launch of the 'No One Walks Alone' protocol in 2015, there was a temporary decrease in falls, but rates have since increased, leading to Presbyterian Hospital exceeding the national average for falls with hip fractures. The model estimates potential return on investment based on interventions to reduce falls, suggesting that targeted strategies can yield significant cost savings and improved patient safety.