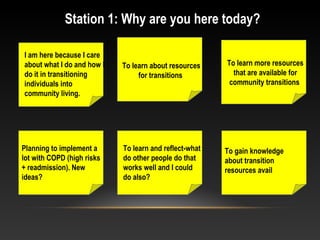
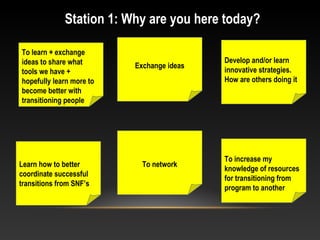
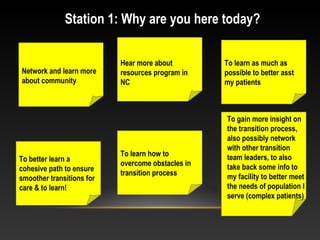
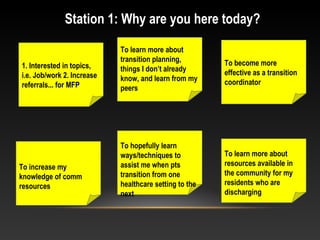
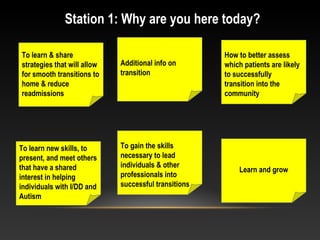
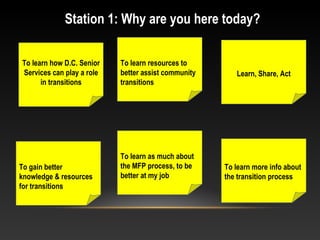
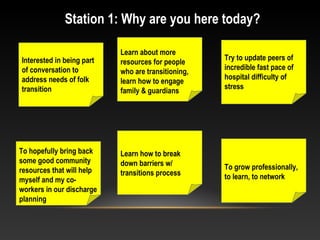
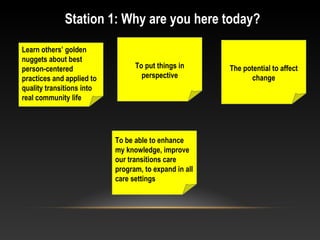
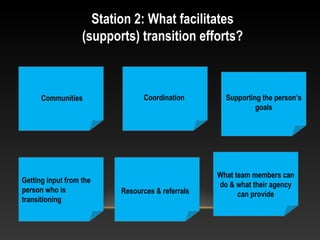
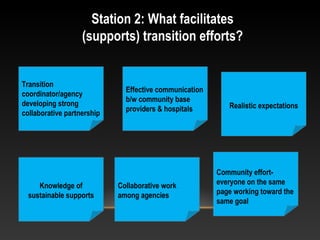
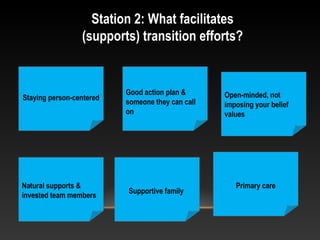
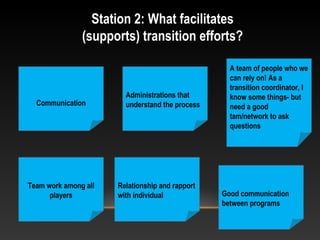
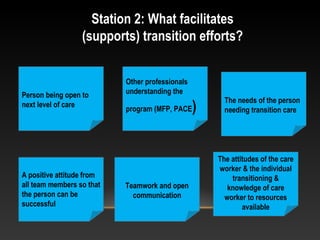
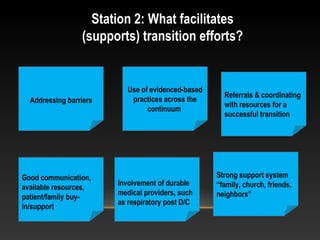
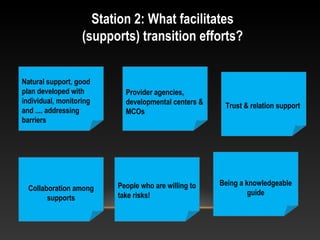
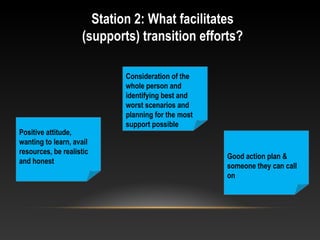
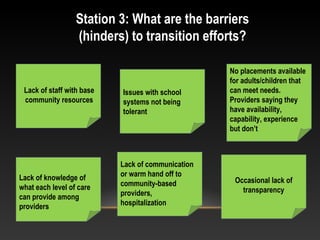
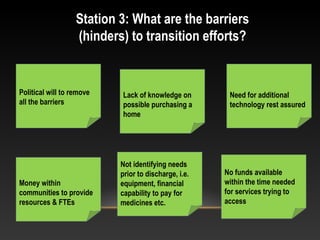
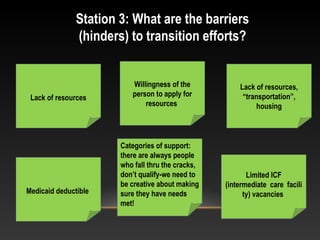
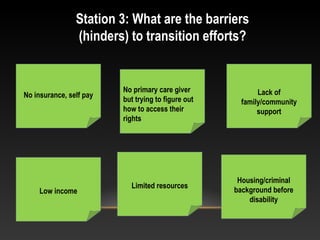
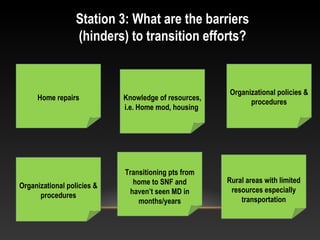
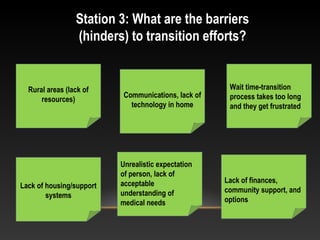
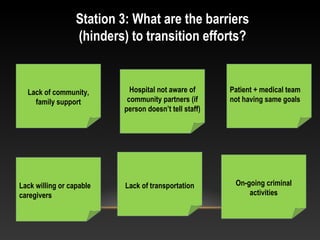
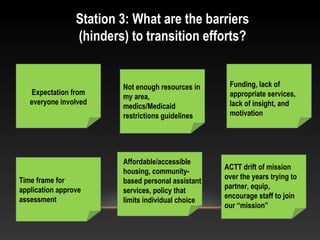
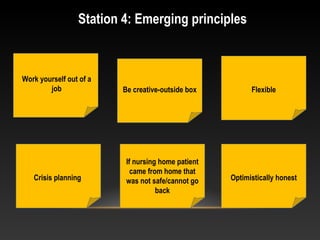
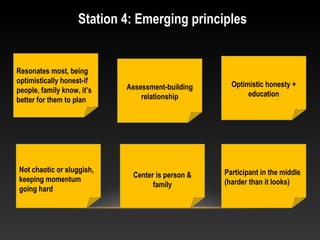
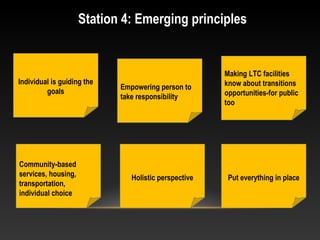
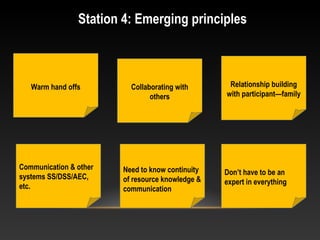
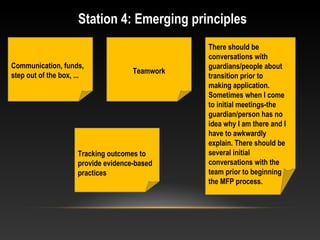
Several attendees shared why they were at the event. Common reasons included wanting to learn about new resources for transitioning individuals, exchange ideas with others, and gain knowledge to help facilitate smoother transitions. When asked what supports successful transitions, many cited good communication between teams, addressing the individual's goals, and having a supportive system in place. Barriers mentioned were lack of resources like housing and transportation, limited availability of community services, and lack of communication between facilities and community providers. Emerging principles discussed were keeping the individual and family's needs and goals at the center, being creatively flexible, and providing optimistically honest information.