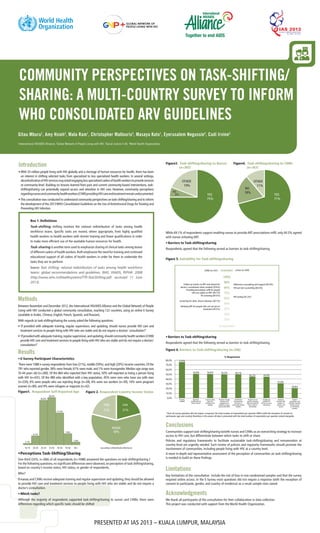
This document summarizes the results of a global survey on community perspectives regarding task-shifting of HIV services from doctors to nurses and community health workers. The survey received responses from over 1000 people in 122 countries. While most respondents supported task-shifting if nurses and health workers received proper training, their views differed on which specific tasks should be shifted. Respondents identified lack of training, inadequate pay, and unsupportive policies as barriers to effective task-shifting. The survey provided insights into community acceptance of task-shifting but had limitations due to its online format and non-random sampling.