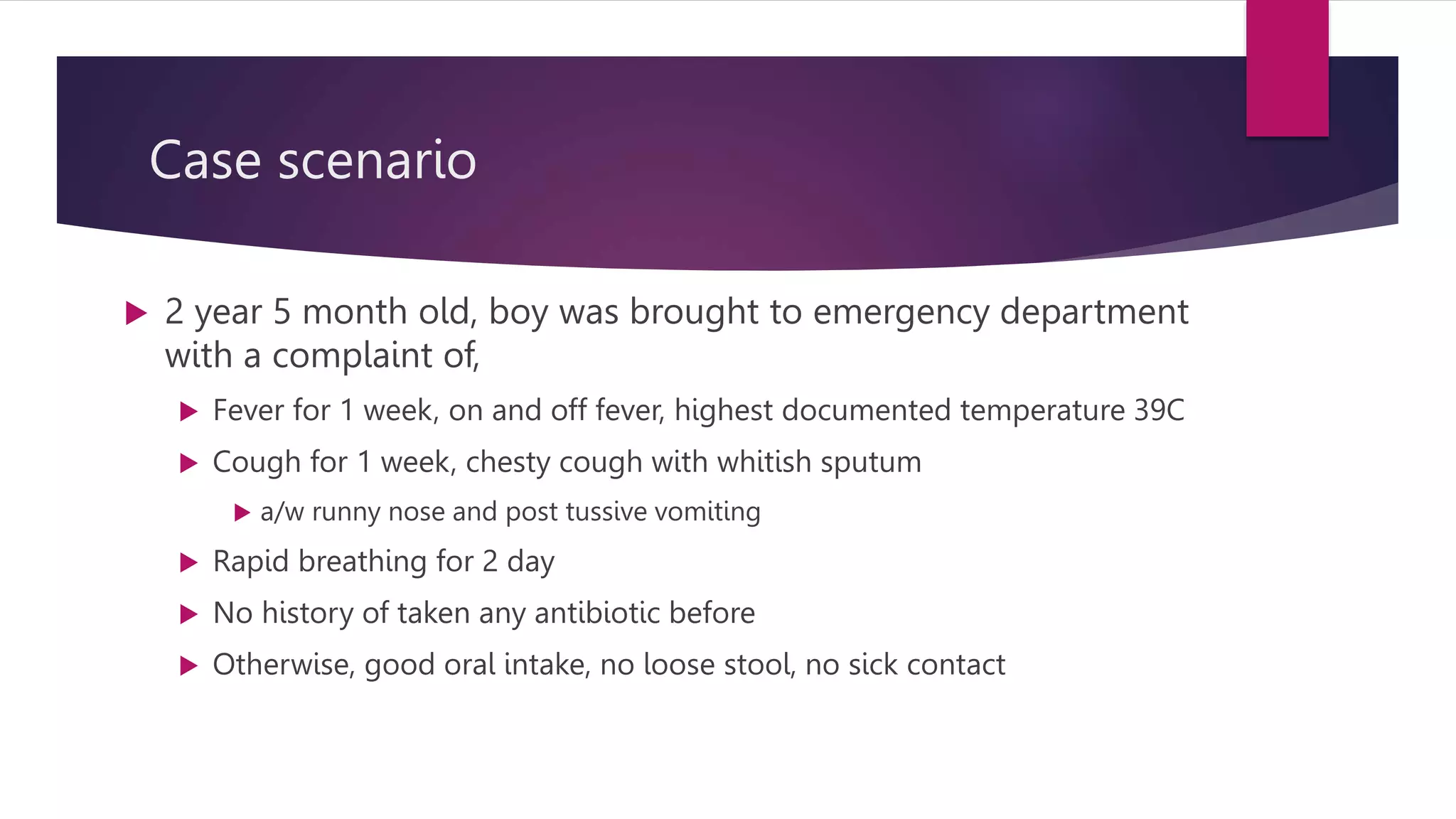
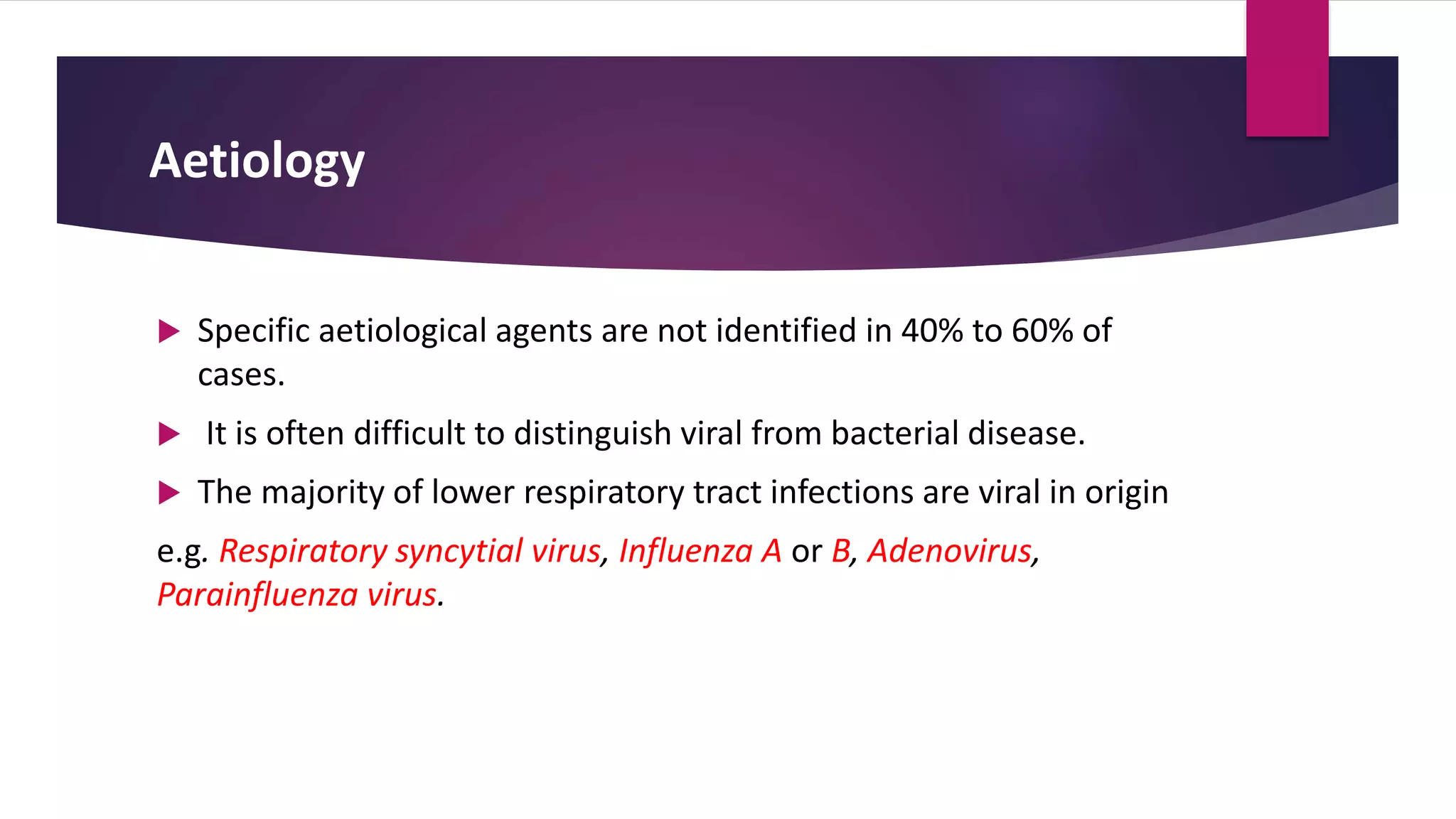
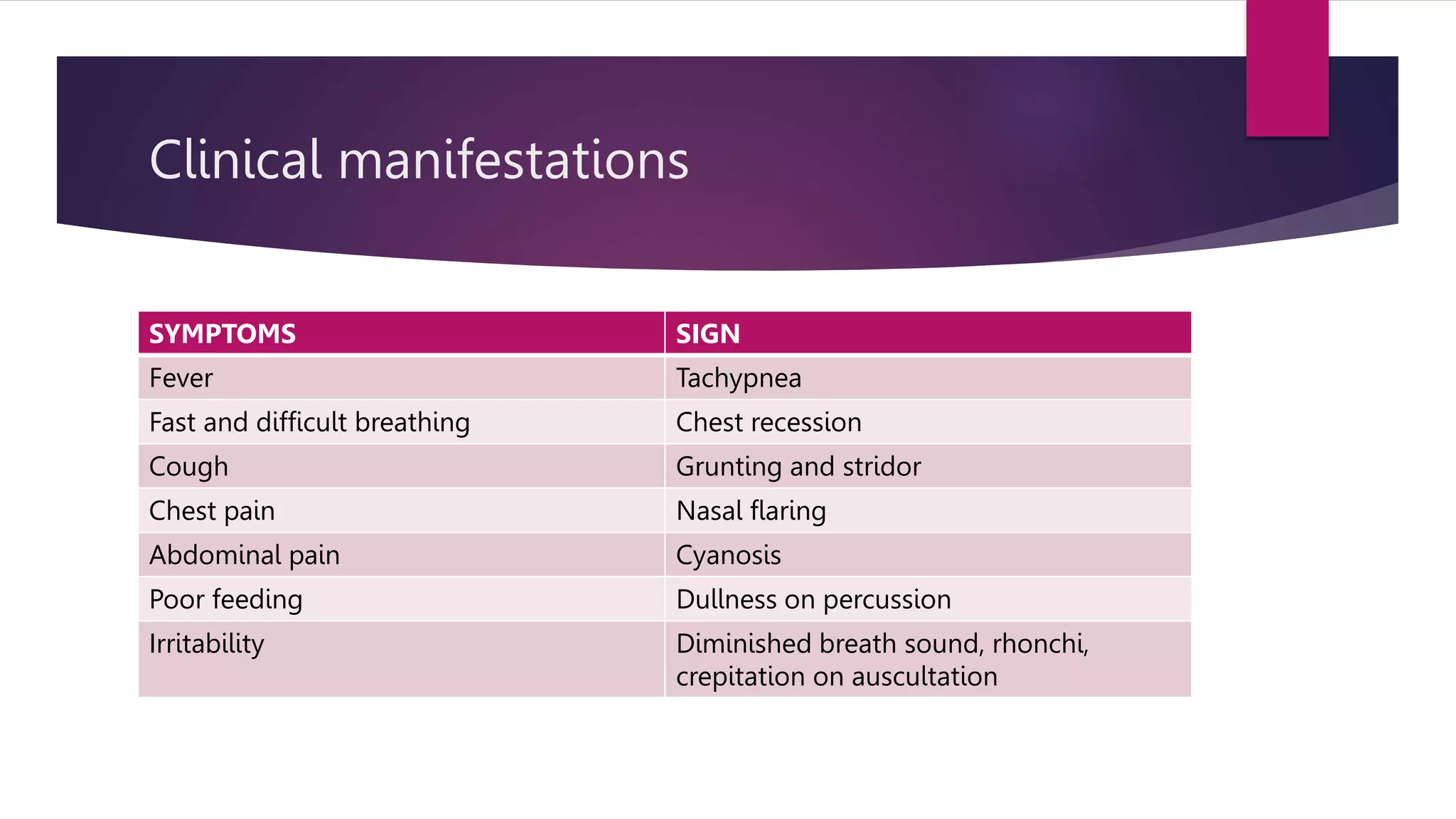
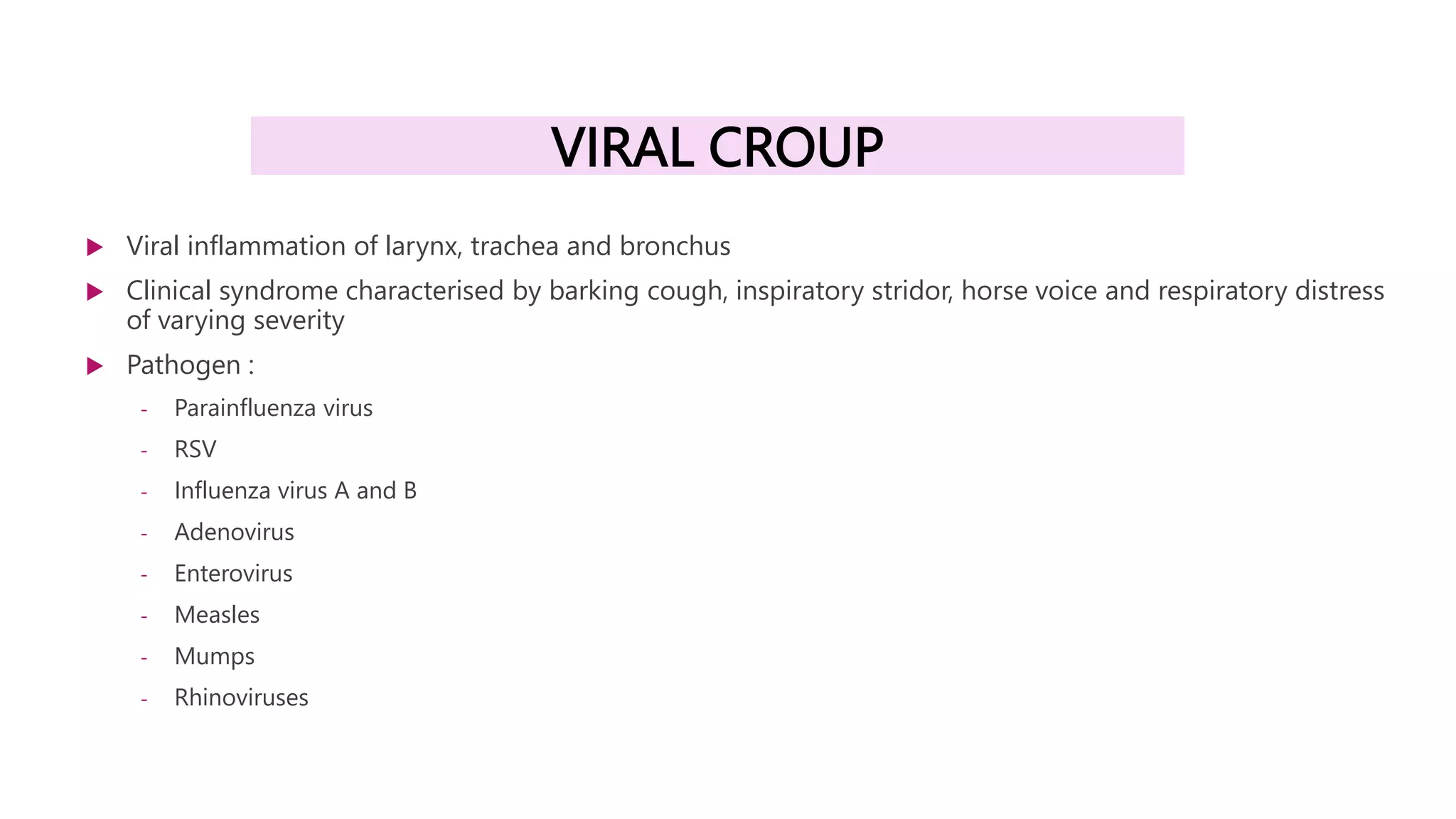
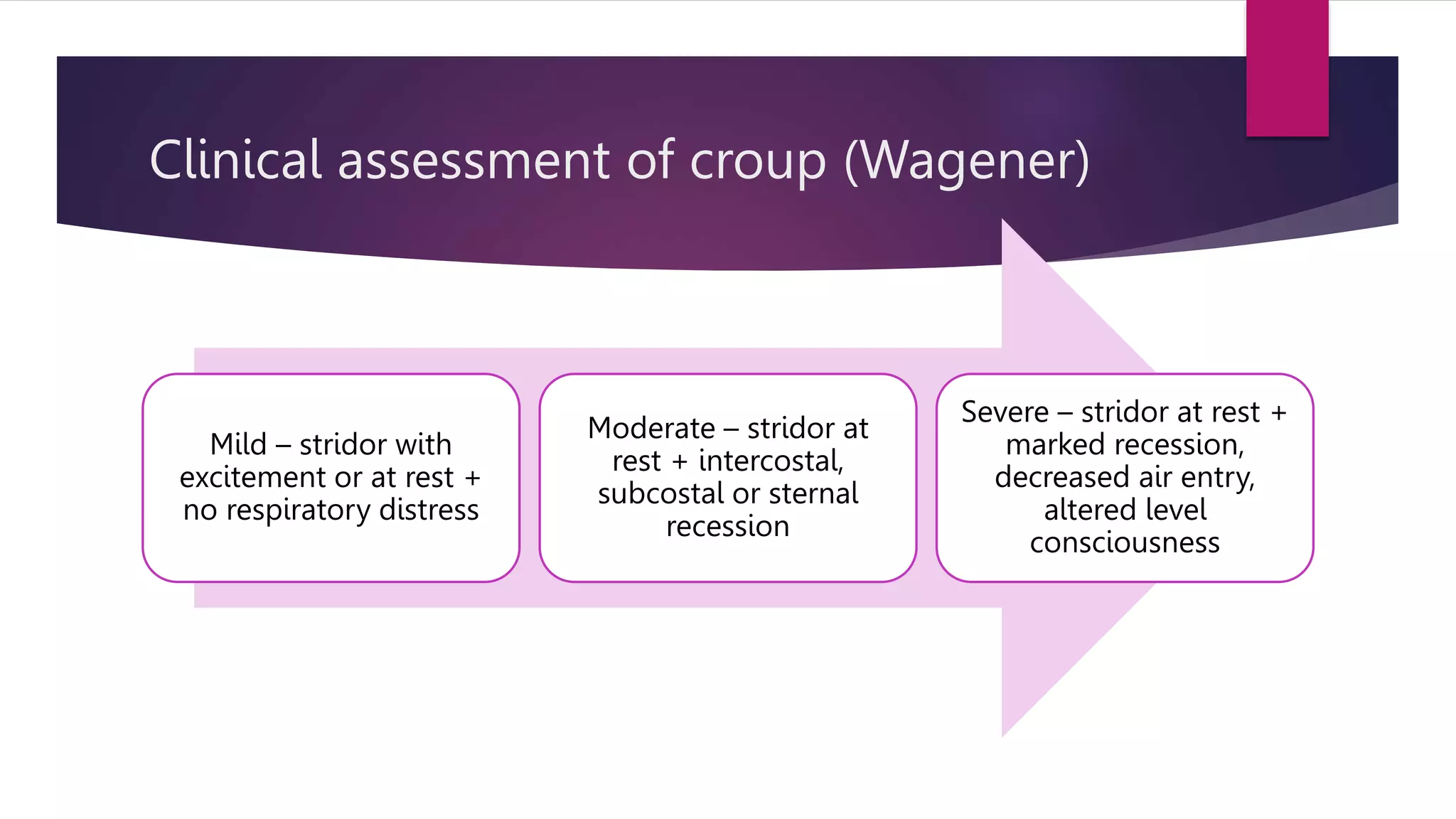
This document provides information on acute respiratory infections including pneumonia, viral bronchiolitis, viral croup, and pertussis. It describes the clinical presentation, diagnostic criteria, and management guidelines for each condition. For pneumonia, it outlines the definitions, common causes, symptoms and signs, criteria for hospitalization, and appropriate antibiotic treatment. Viral bronchiolitis is commonly caused by RSV and presents with tachypnea, wheezing, and respiratory distress in infants. Viral croup presents with a barking cough, inspiratory stridor, and respiratory distress that varies in severity. Pertussis causes paroxysmal coughing fits accompanied by a whoop.