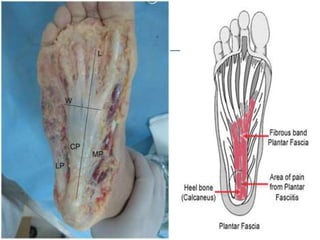
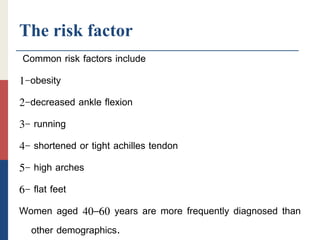
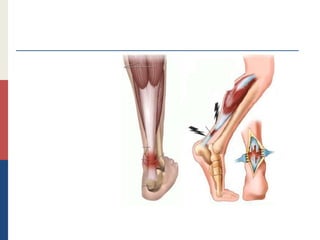
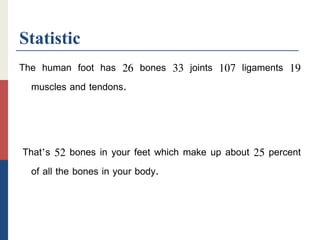
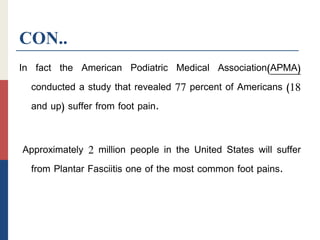
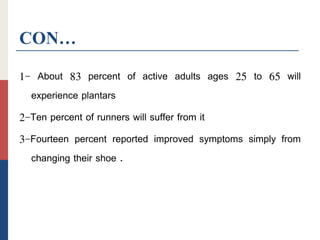
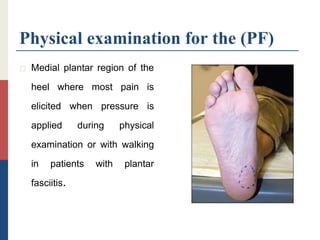
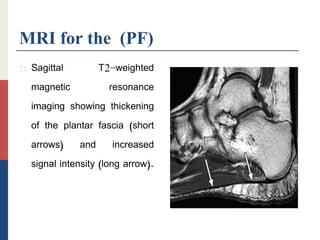
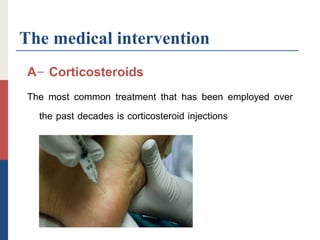
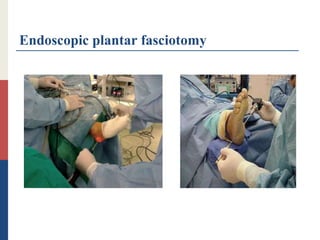
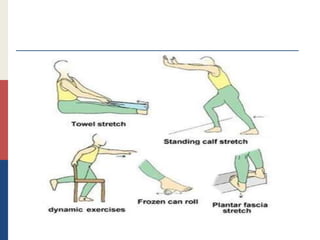
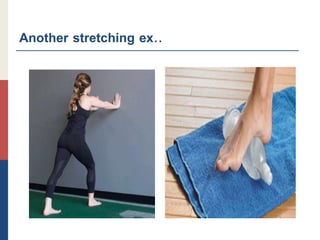
This document summarizes information about planter fasciitis, including its definition, symptoms, diagnosis, and treatment options. Planter fasciitis is a common cause of heel pain resulting from repetitive microtrauma to the plantar fascia. It is diagnosed based on symptoms of pain in the heel worsened by activity and improved by rest. Treatment includes medical management with corticosteroid injections, physical therapy focusing on stretching and strengthening exercises, and surgery as a last resort.