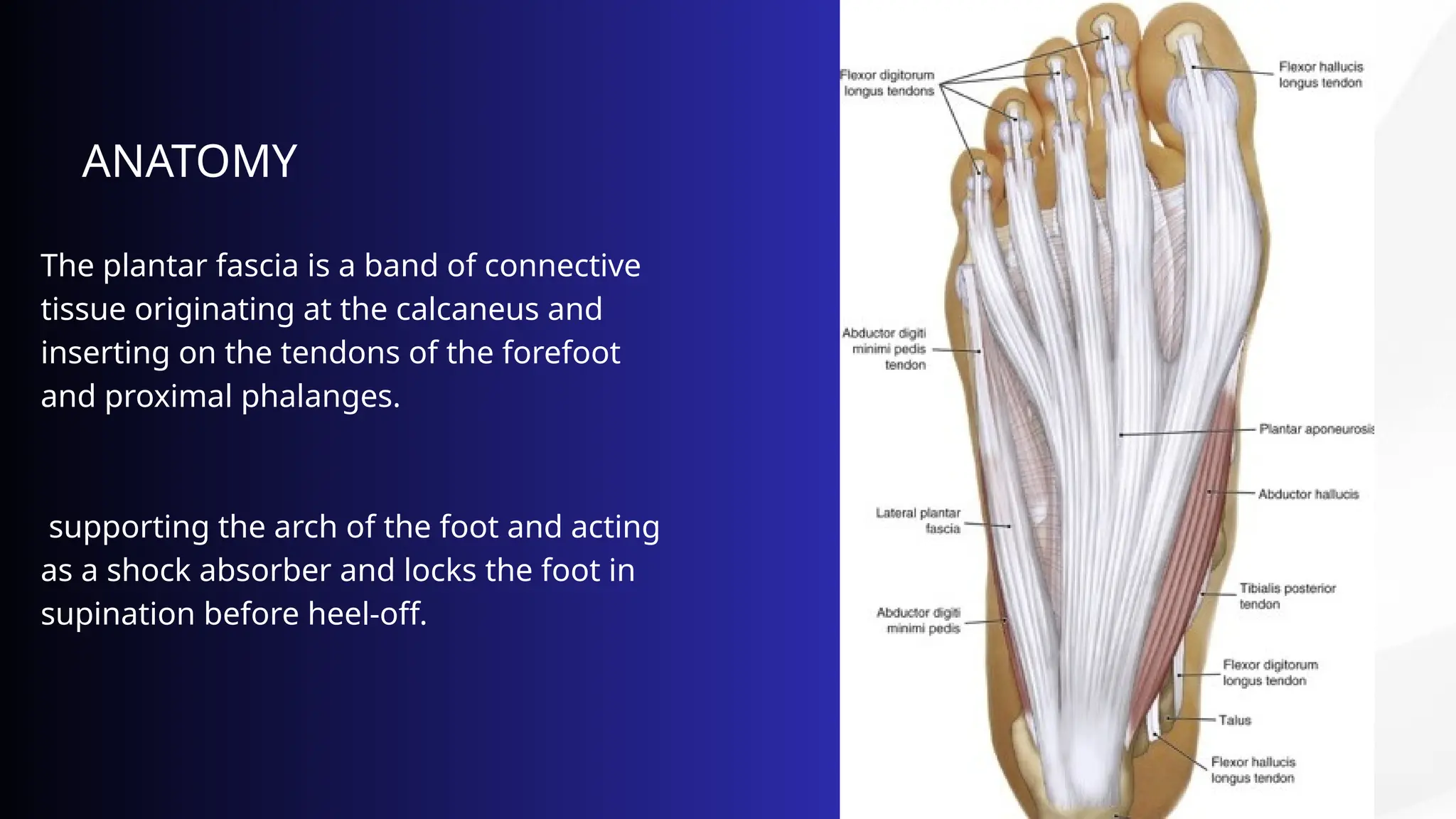
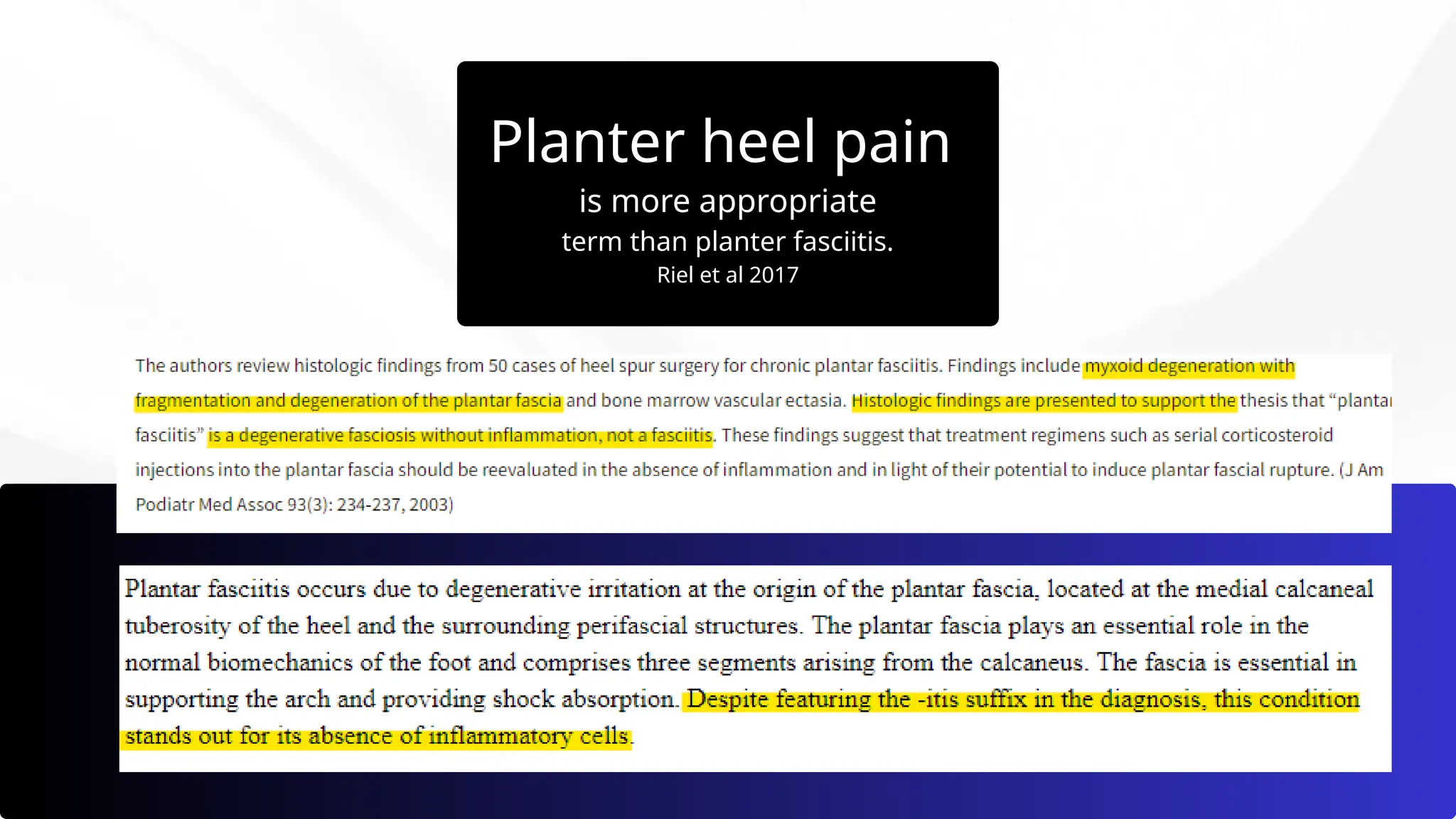
Plantar fasciitis, or plantar heel pain, is a degenerative condition of the plantar fascia due to repetitive microtears, often resulting from multifactorial causes such as flat feet or improper footwear. Patients typically experience morning pain that alleviates with movement, and the diagnosis is primarily clinical, with ultrasound helping to confirm the condition. Conservative treatments are effective for 70-80% of patients, and surgery may be considered if pain persists after 12 months of non-surgical management.