This document provides information on occupational exposure prophylaxis (PEP) for HIV. It discusses:
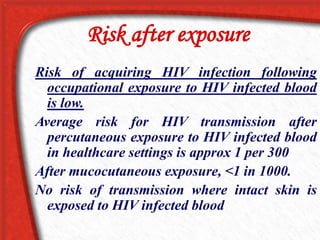
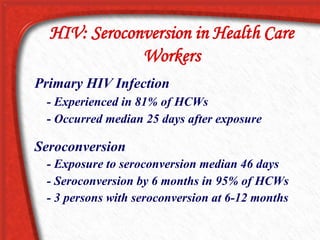
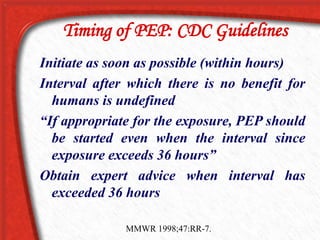
1. The risk of HIV transmission from occupational exposures is low, estimated at 1 in 300 for a needlestick from a known HIV+ source. PEP using antiretrovirals can reduce this risk up to 81%.
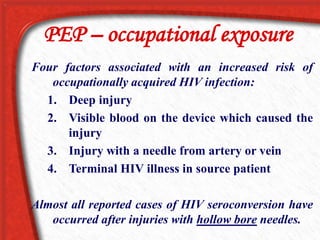
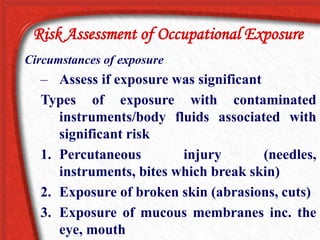
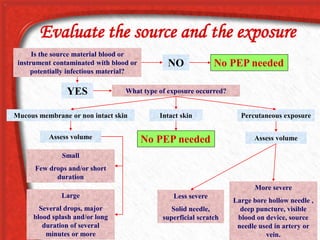
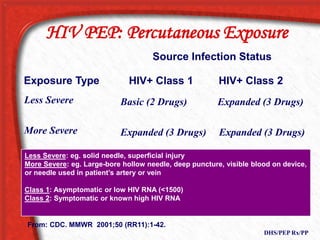
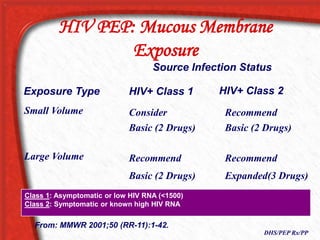
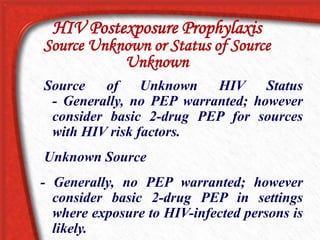
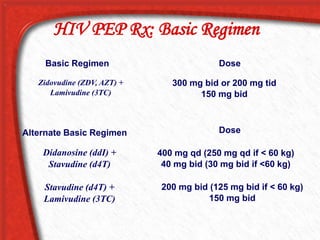
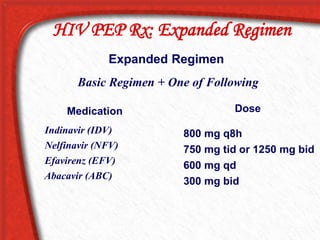
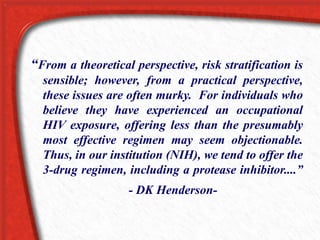
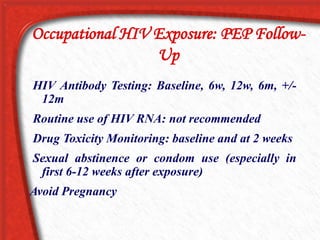
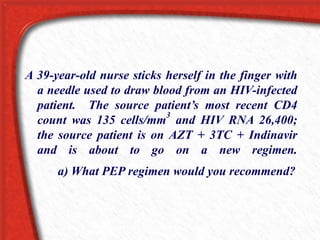
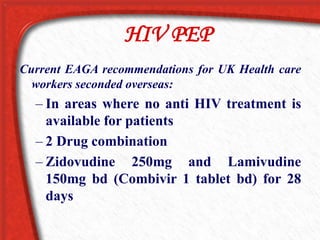
2. PEP treatment recommendations depend on the type of exposure, characteristics of the exposure (e.g. deep injury, visible blood), and characteristics of the source patient (e.g. viral load, antiretroviral treatment). A basic 2-drug regimen is usually recommended but an expanded 3-drug regimen may be used for higher risk exposures.
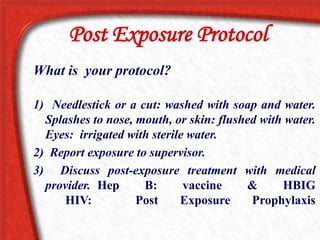
3. Proper wound