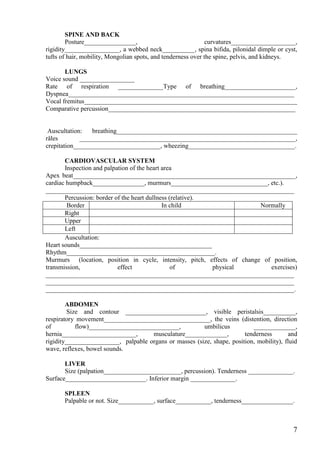
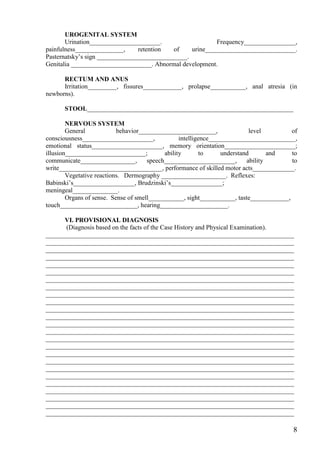
This document contains a student case history form used by the Department of Pediatrics at Kharkov National Medical University. The form includes sections for general patient information, current complaints, medical history of present illness, past medical history including family history and development, and physical exam findings. It requests identifying and demographic information about the patient, as well as detailed information about the patient's health status, symptoms, diagnoses, treatments, and relevant family and social history to provide context for the patient's current medical case.