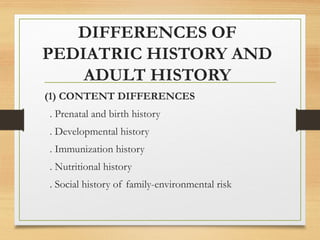
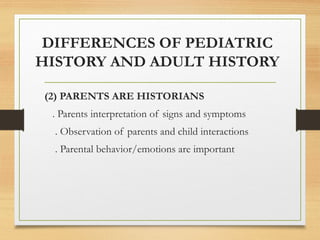
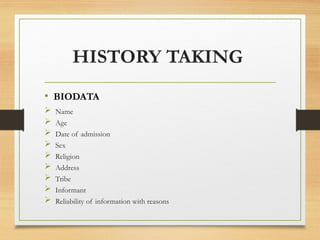
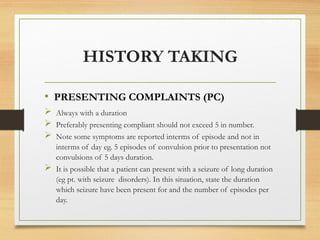
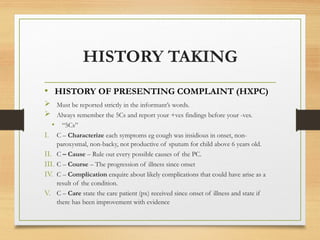
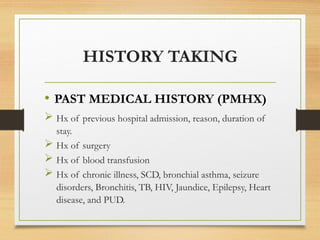
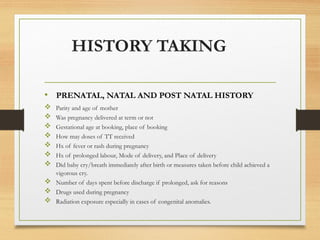
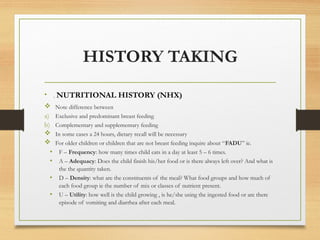
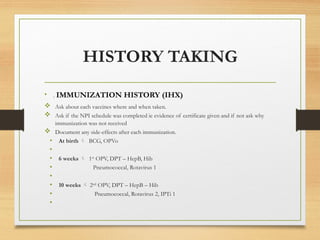
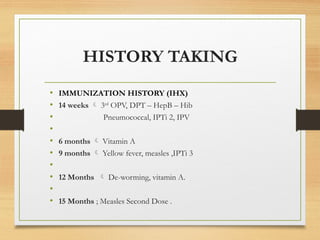
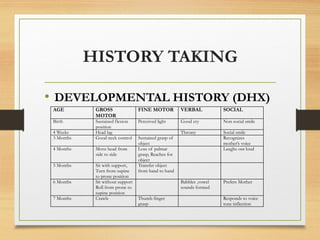
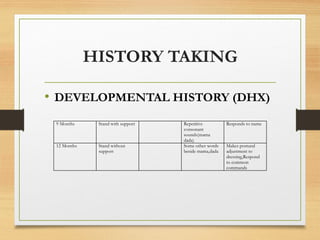
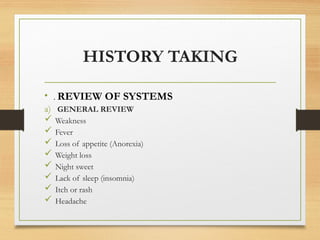
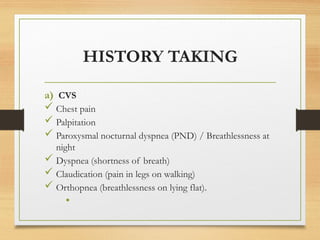
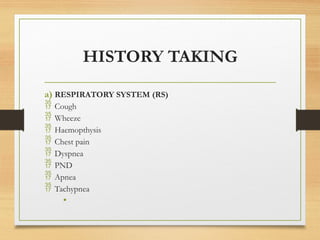
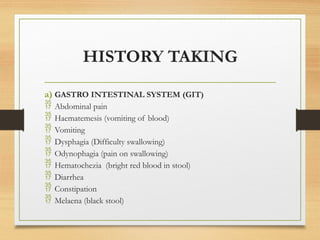
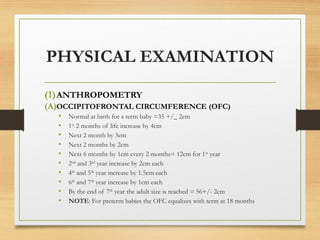
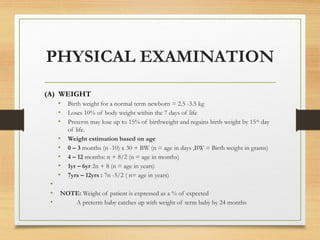
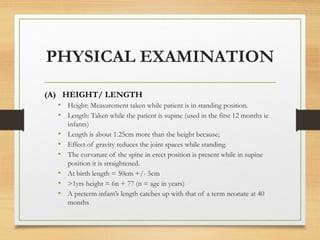
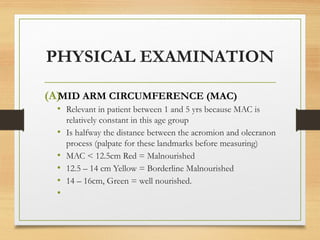
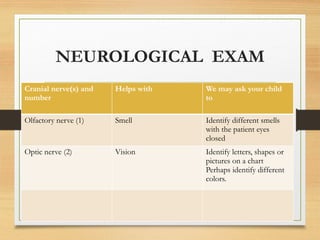
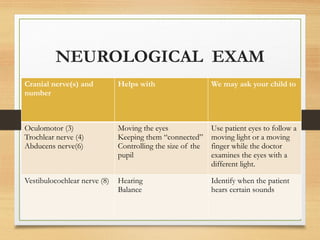
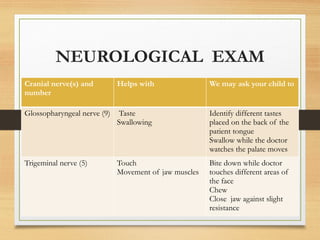
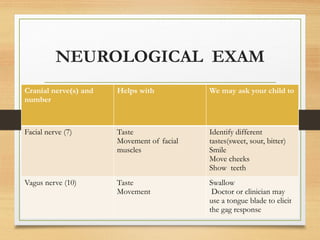
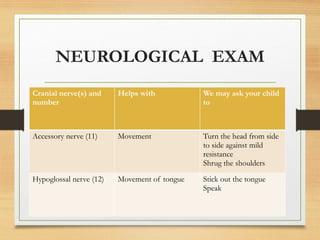
The document outlines the essential steps and considerations for taking a pediatric history and conducting physical examinations in children. It details the differences between pediatric and adult histories, highlighting the importance of parental input and specific histories, including developmental, immunization, and nutritional. Additionally, it provides a comprehensive overview of physical examination components, including anthropometry, systemic examination, and neurological assessments.