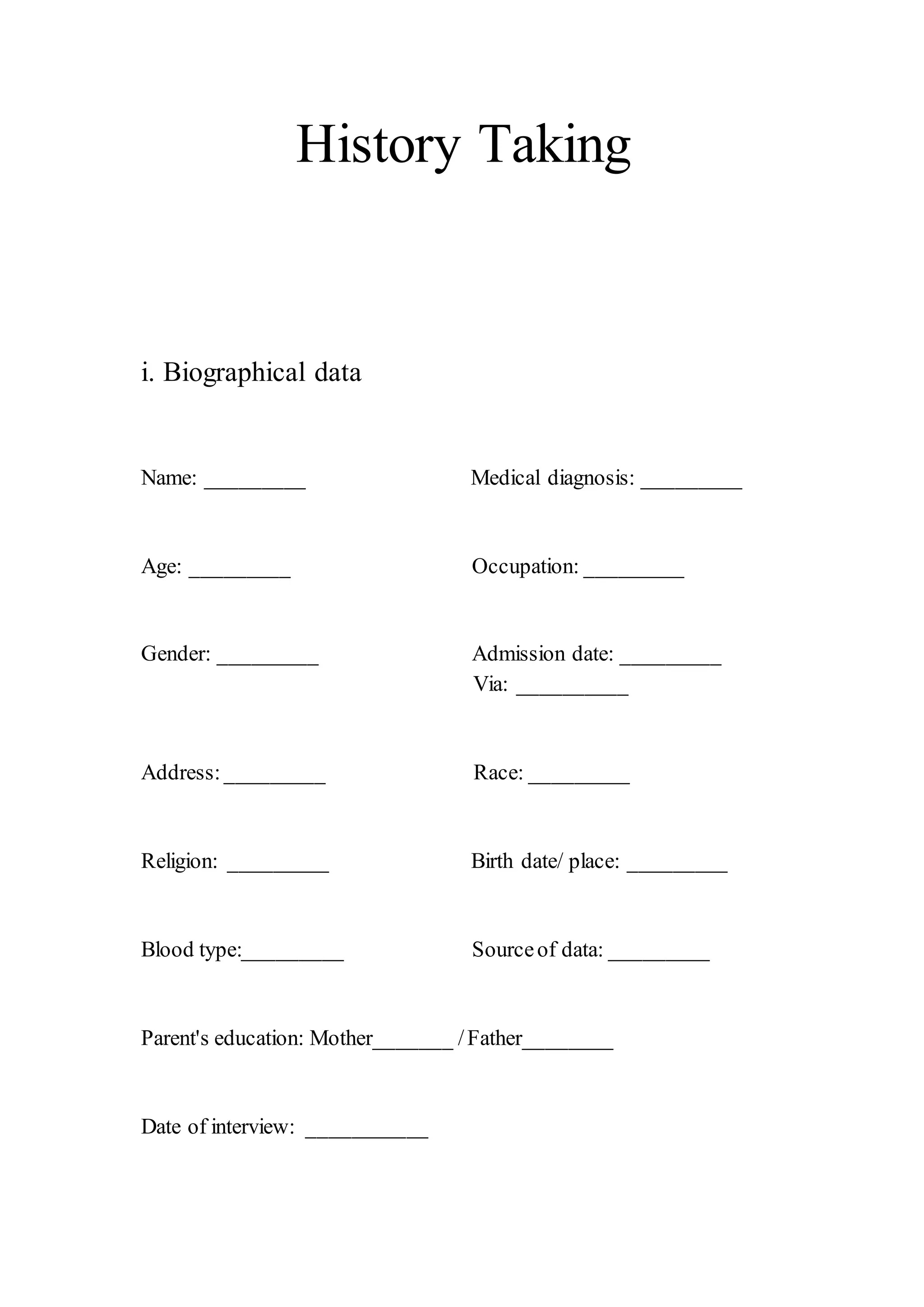
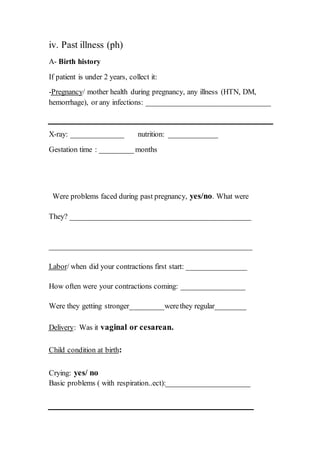
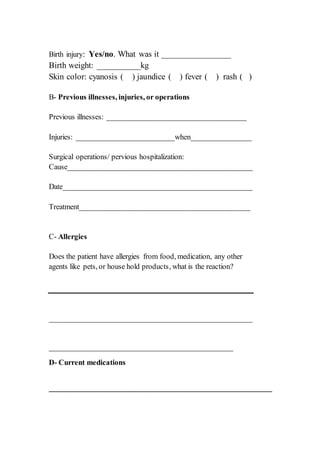
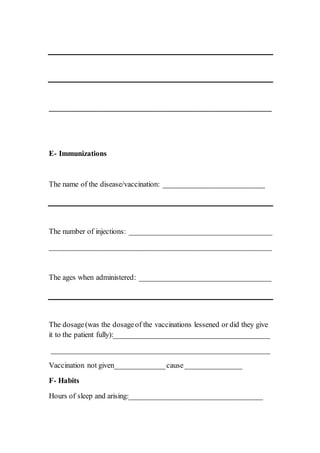
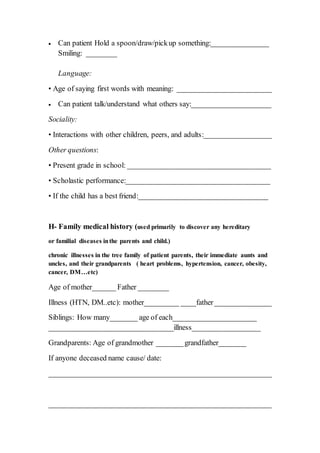
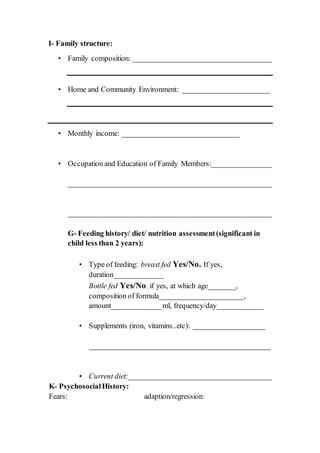
The document is a comprehensive template for conducting a medical history taking that includes sections for biographical data, chief complaint, present illness, past illnesses, allergies, current medications, immunizations, habits, growth and development, family medical history, family structure, feeding history, and psychosocial history. Each section has specific prompts for details such as severity, timing, and associated factors related to the patient's symptoms. This structured format is designed to gather thorough information essential for patient assessment and diagnosis.