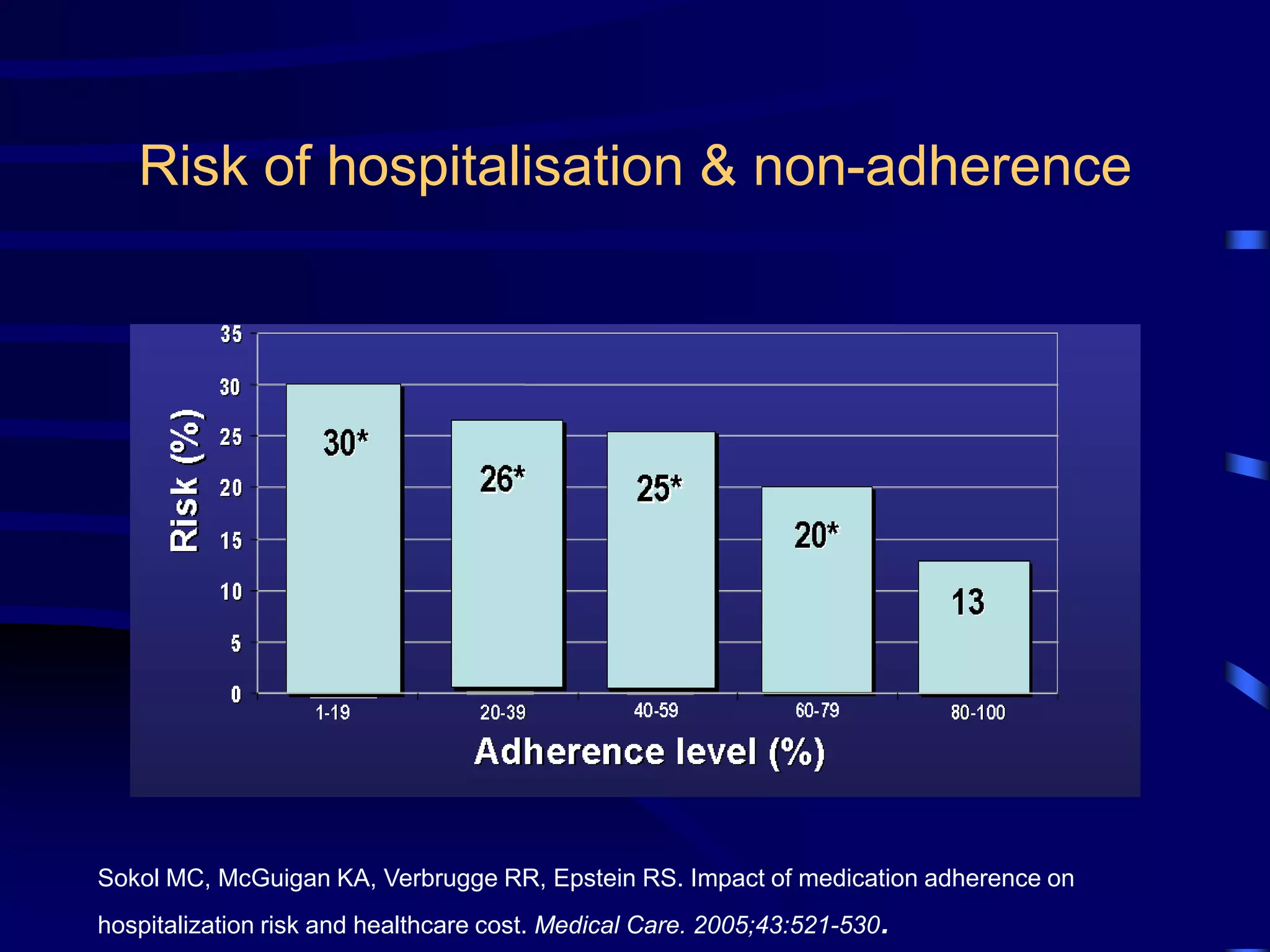
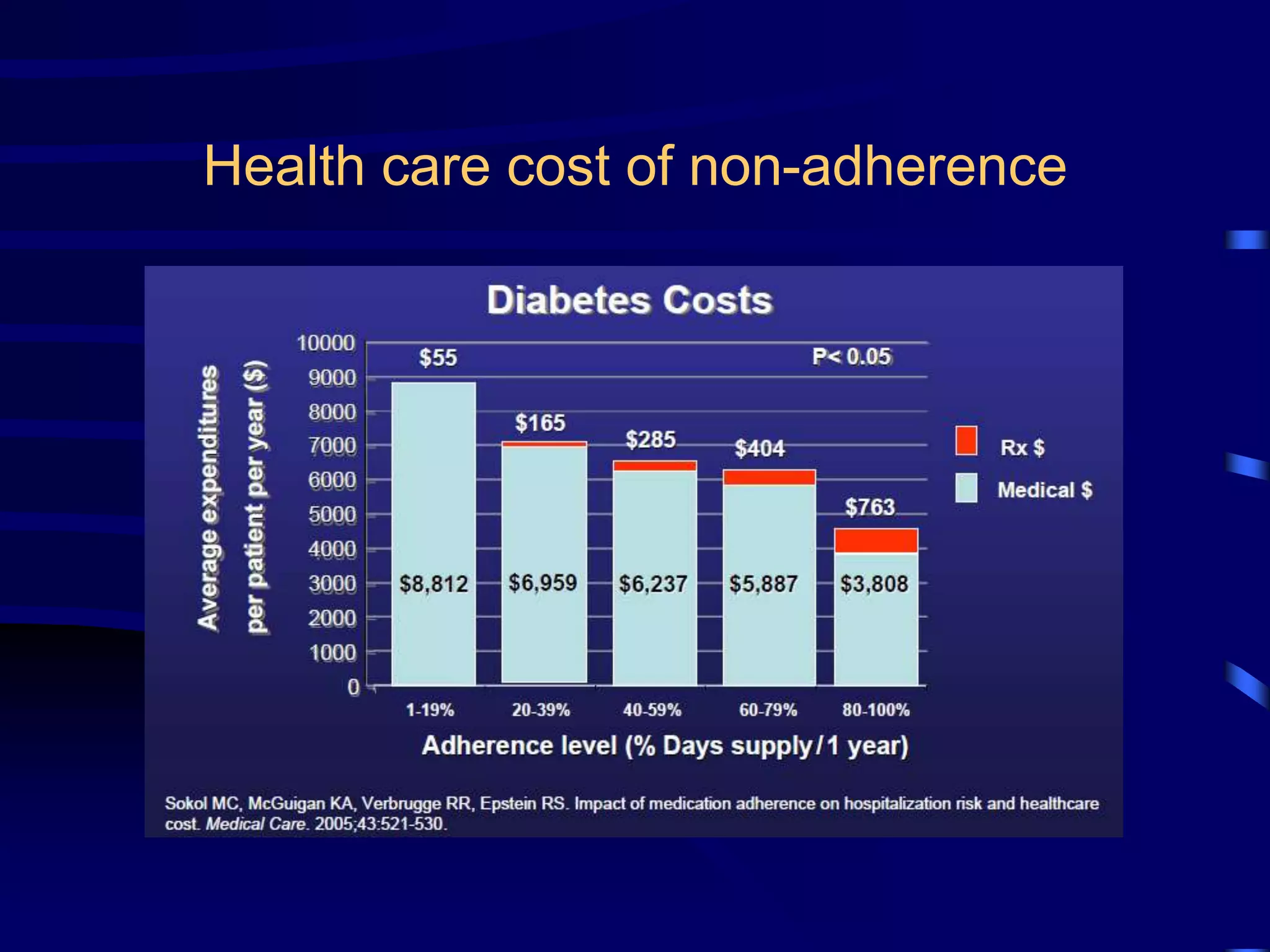
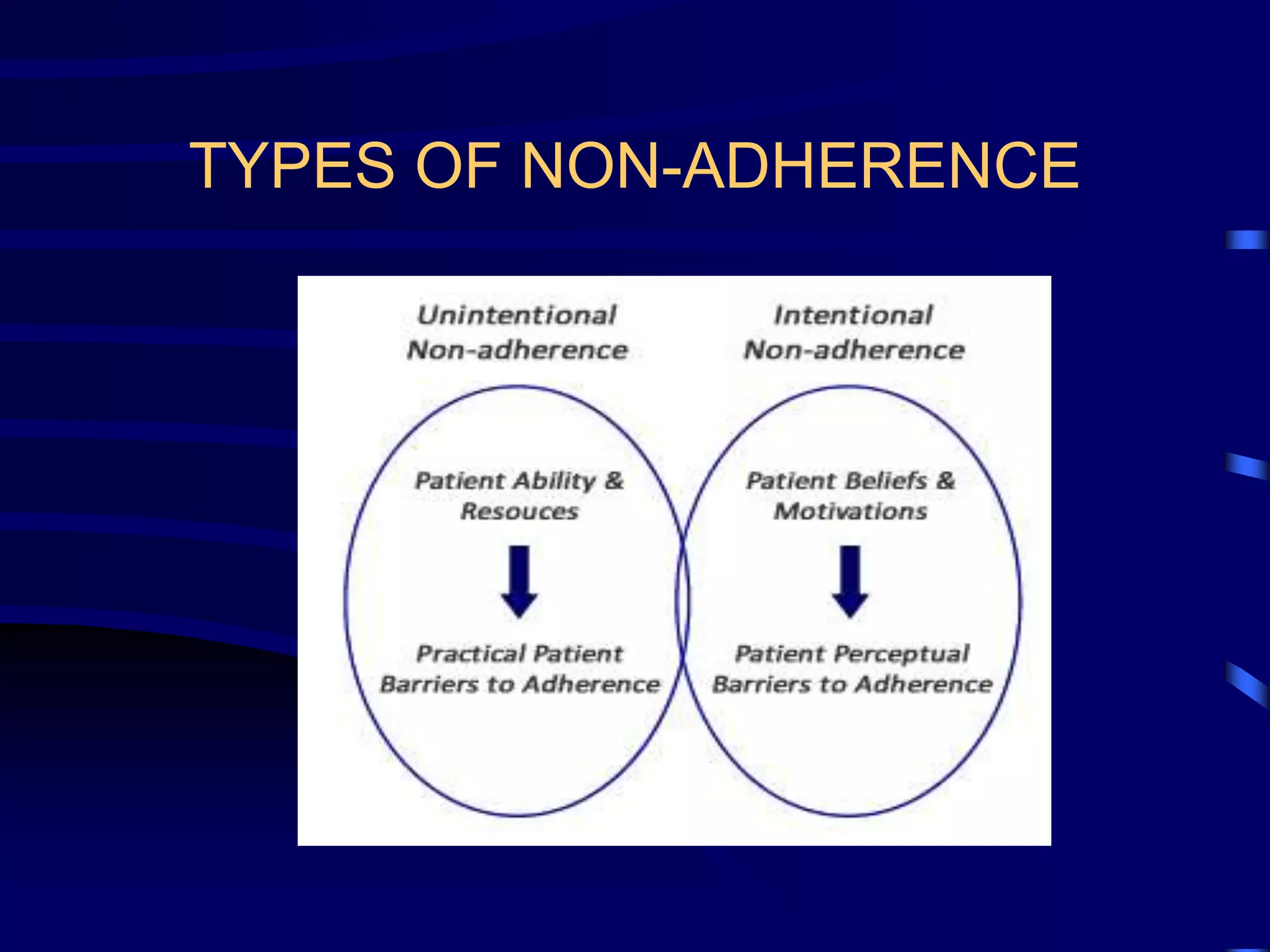
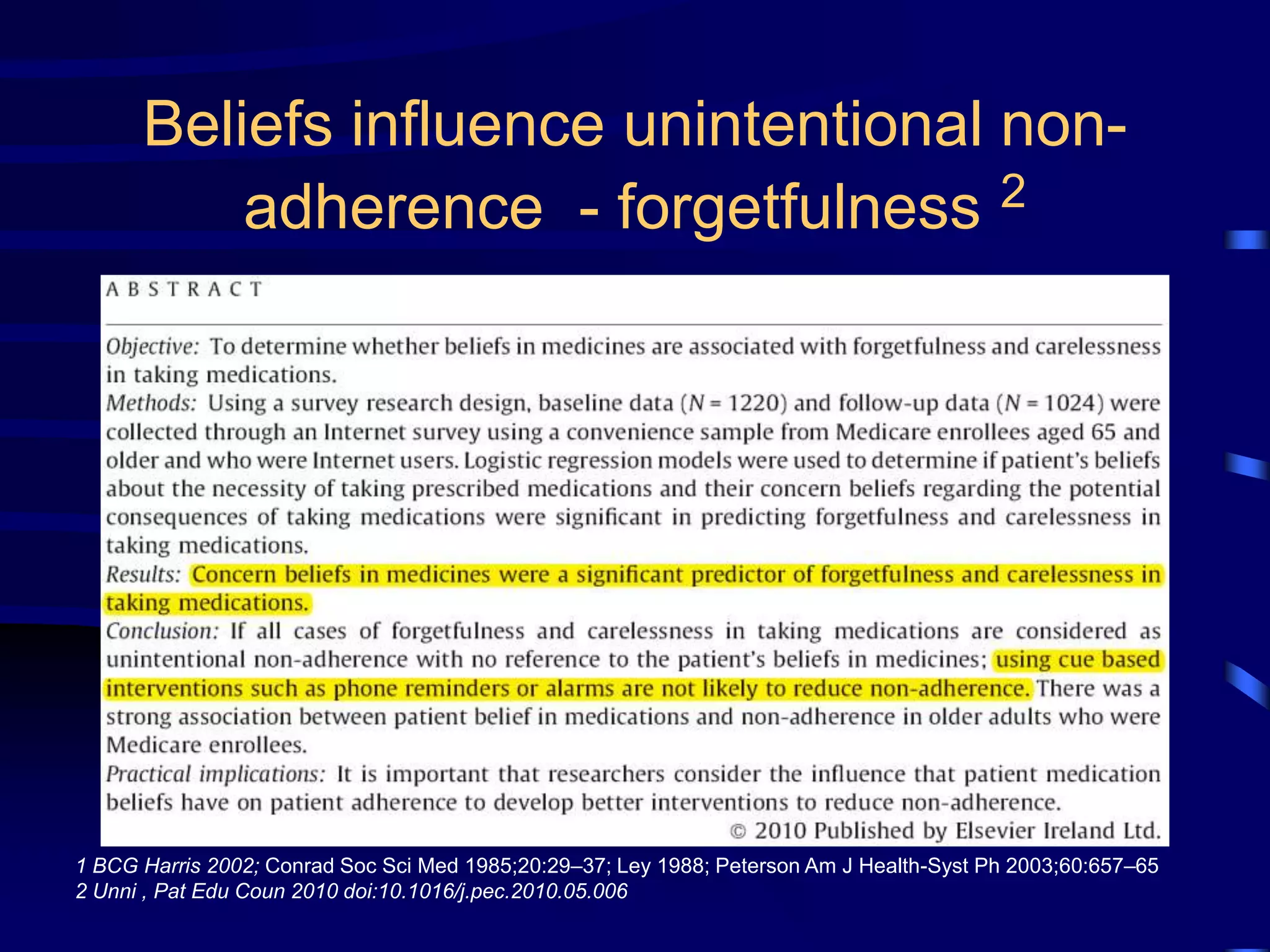
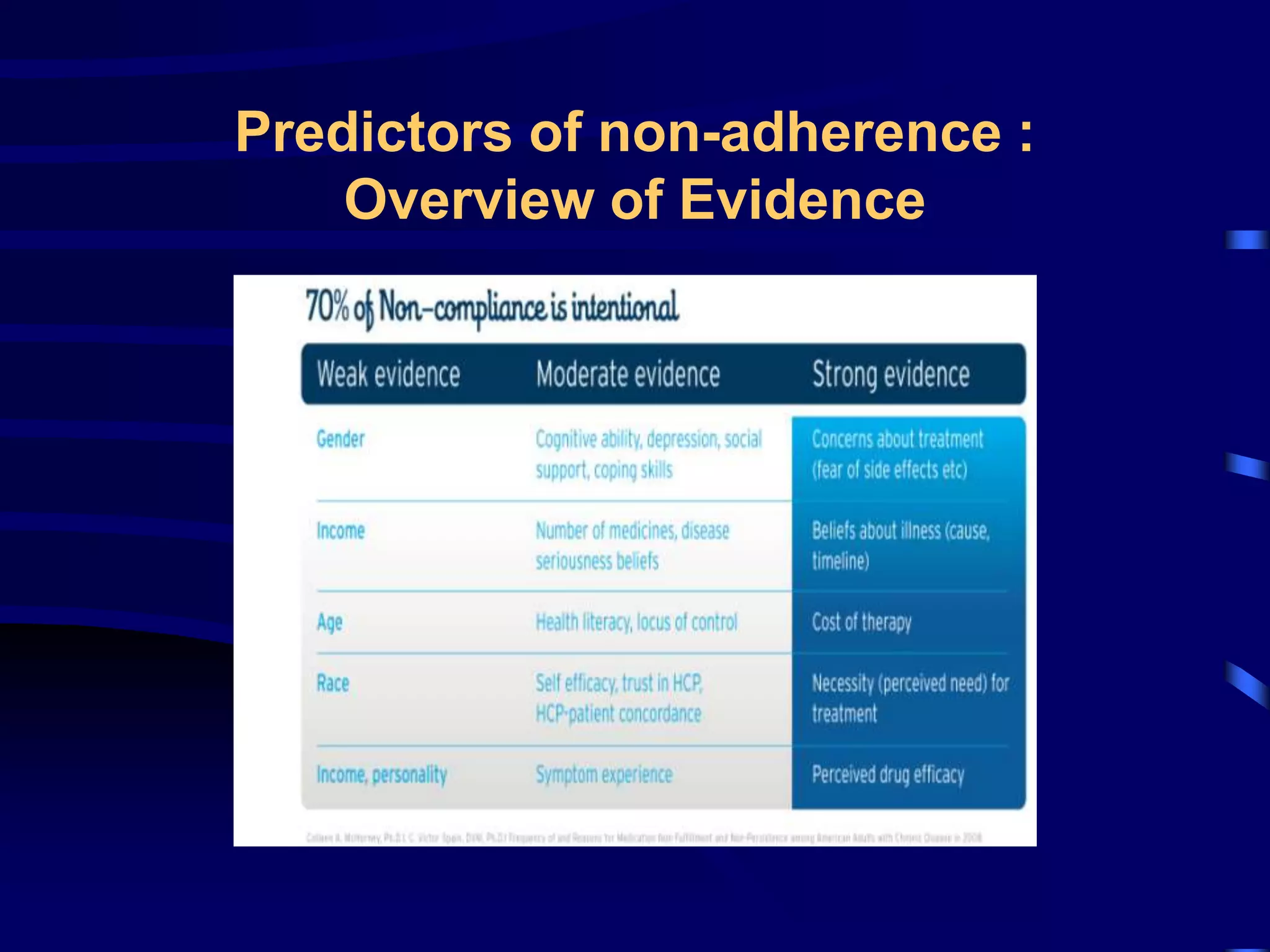
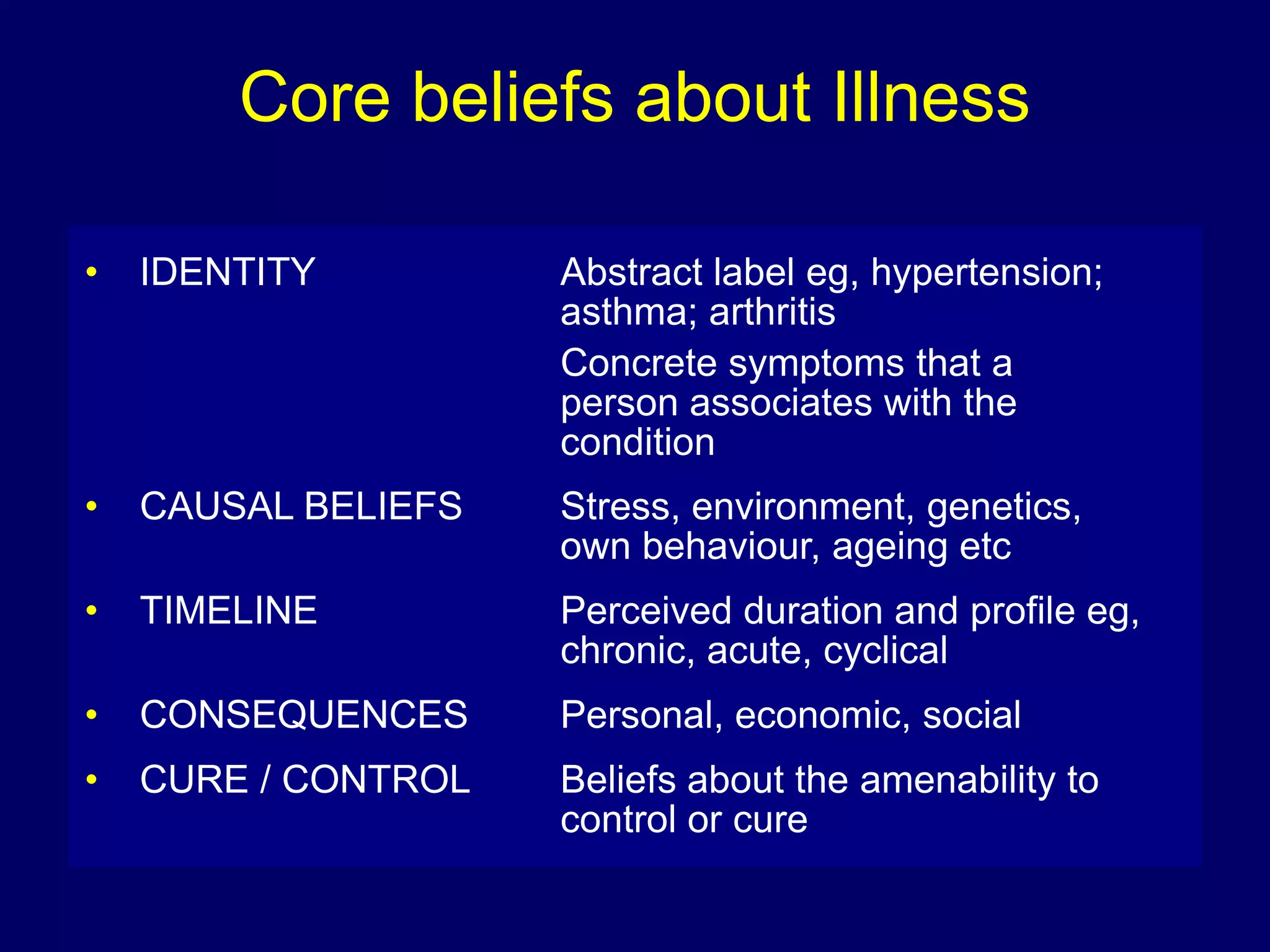
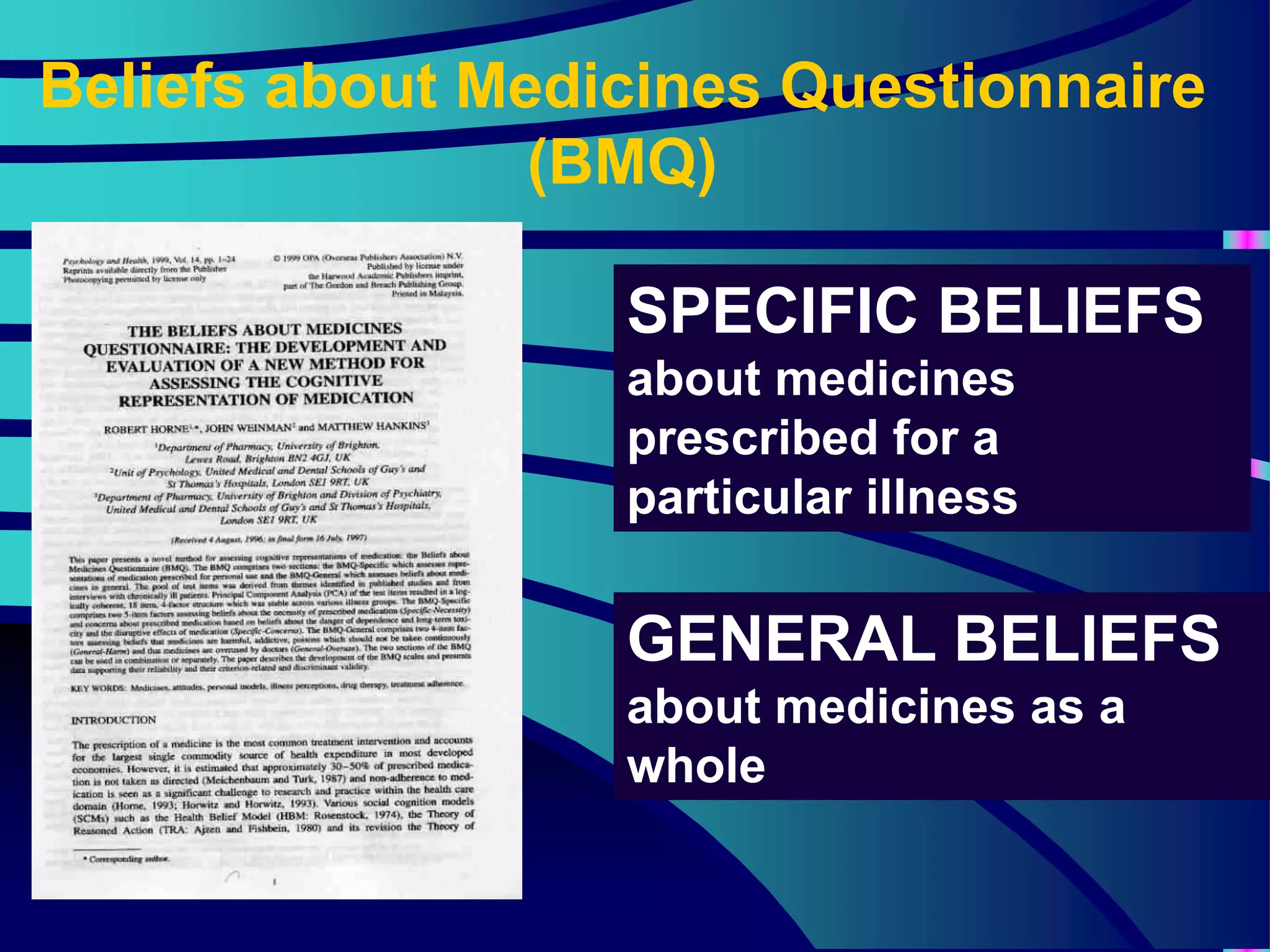
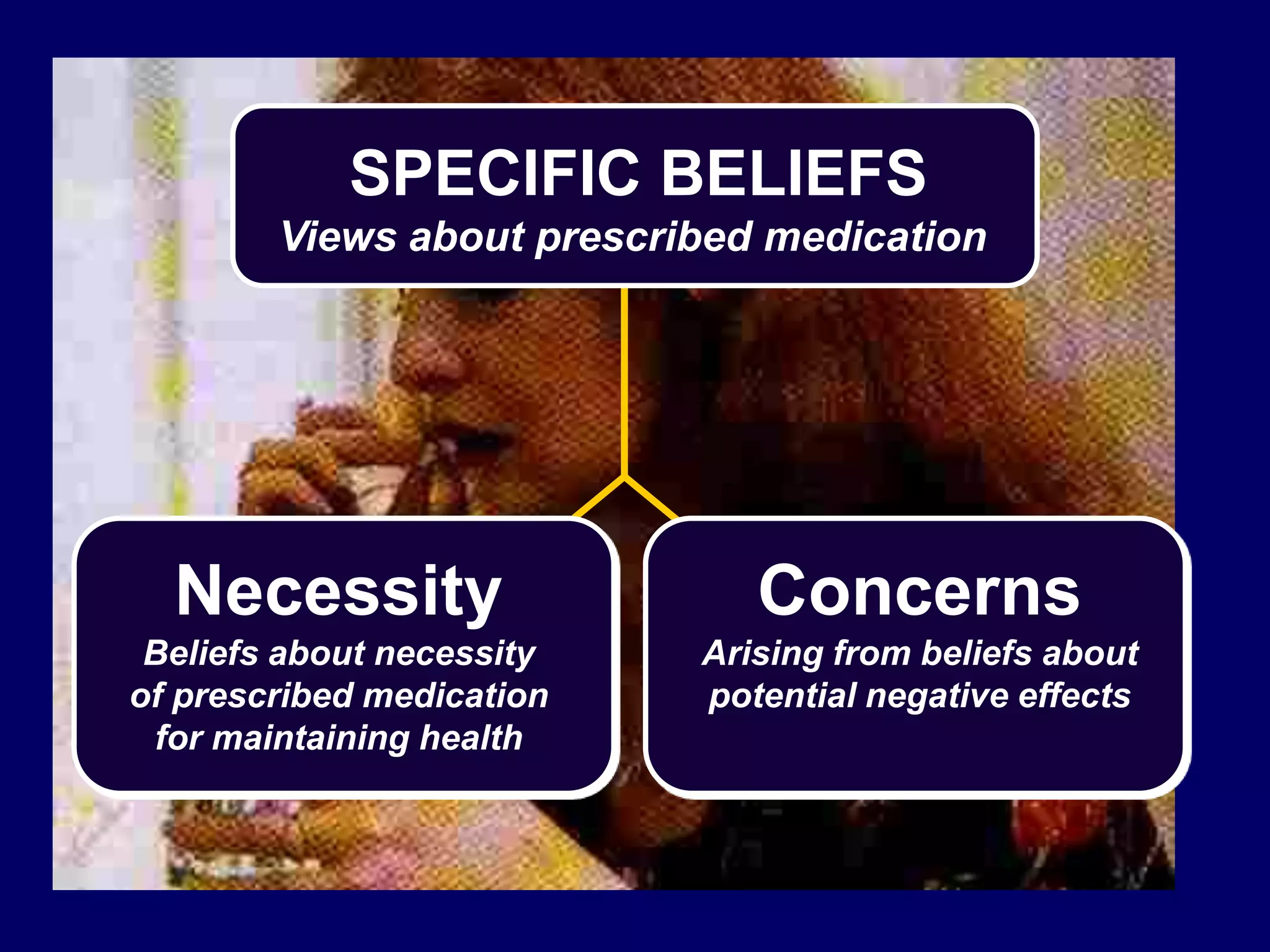
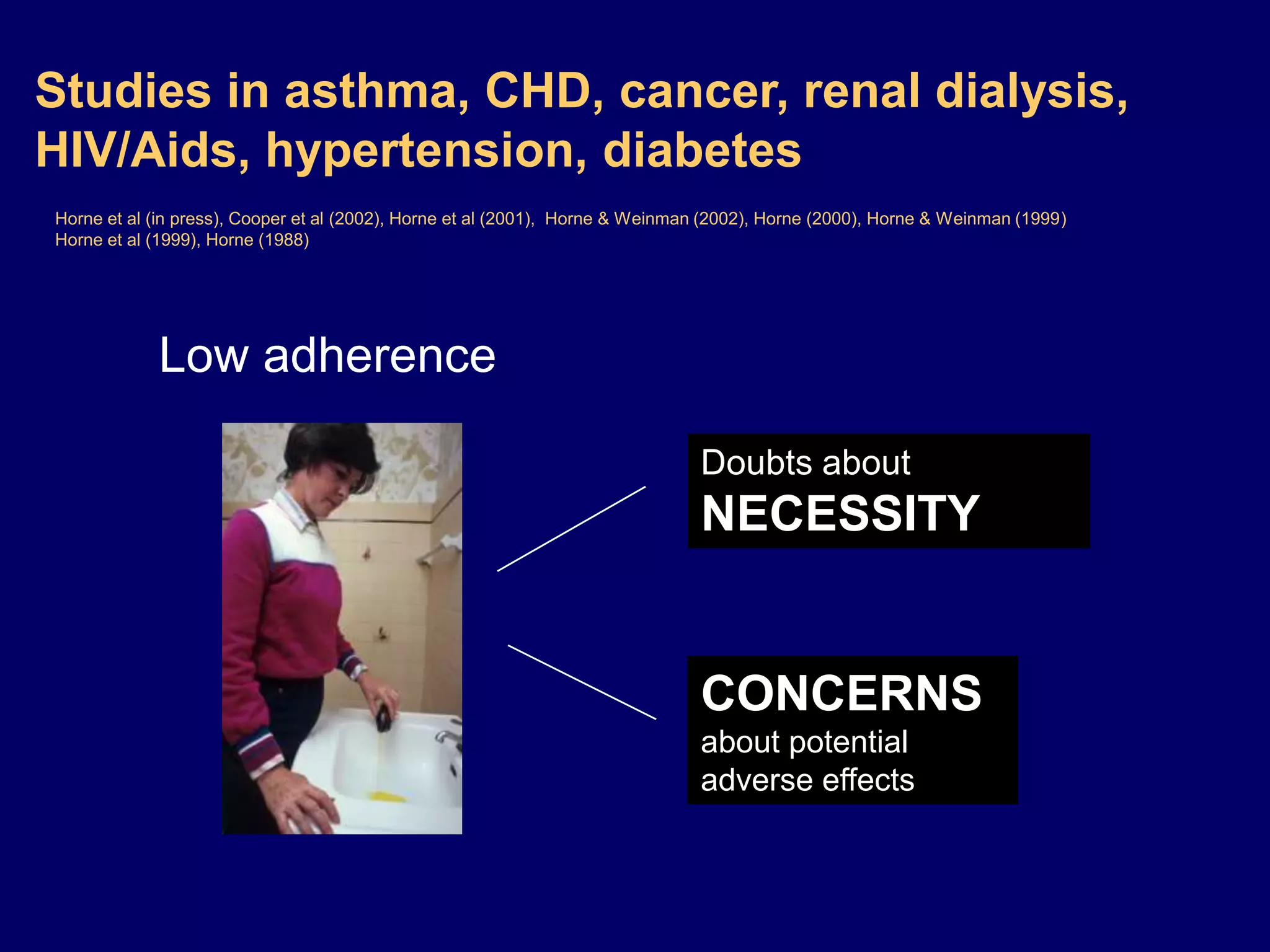
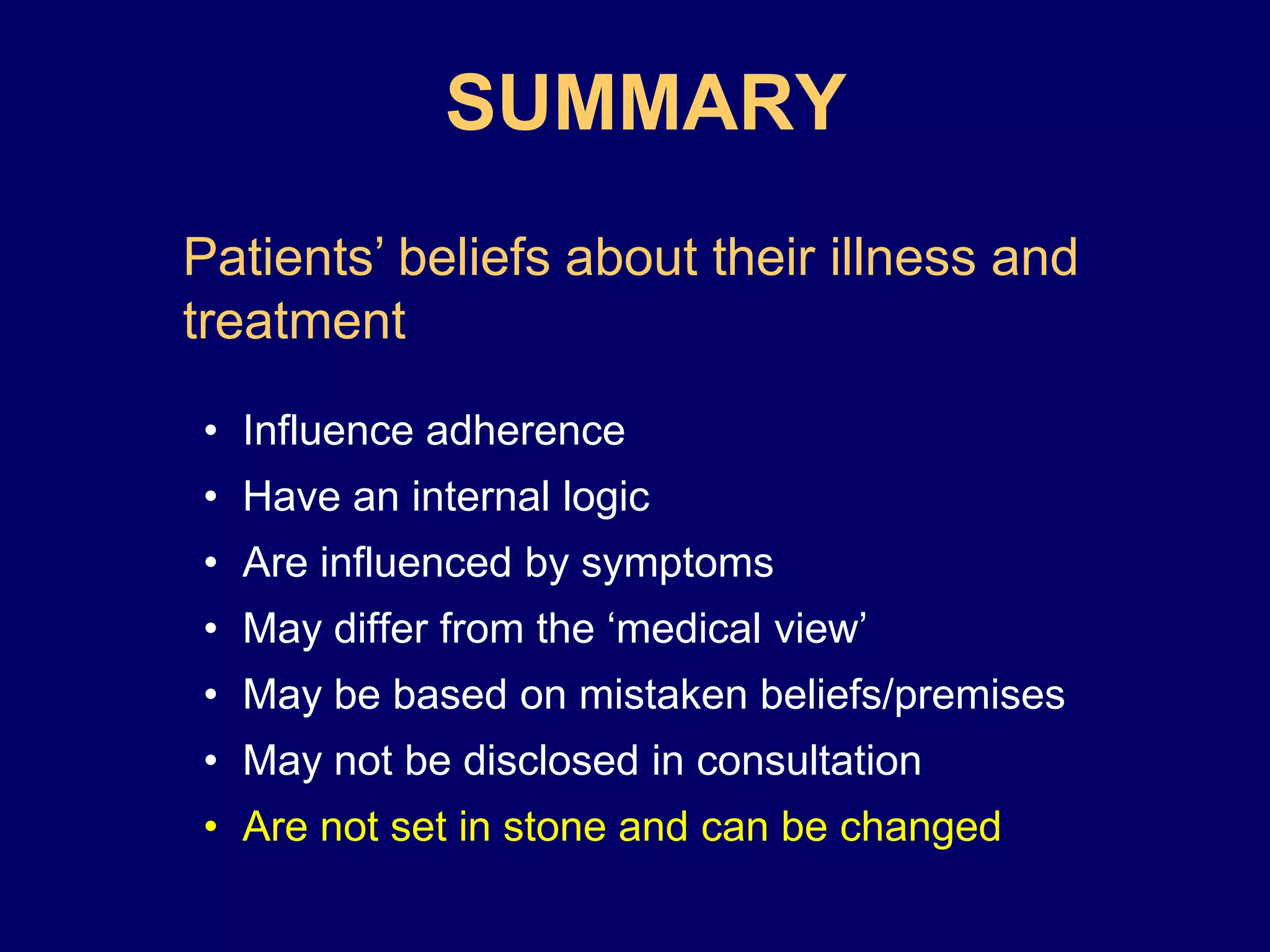
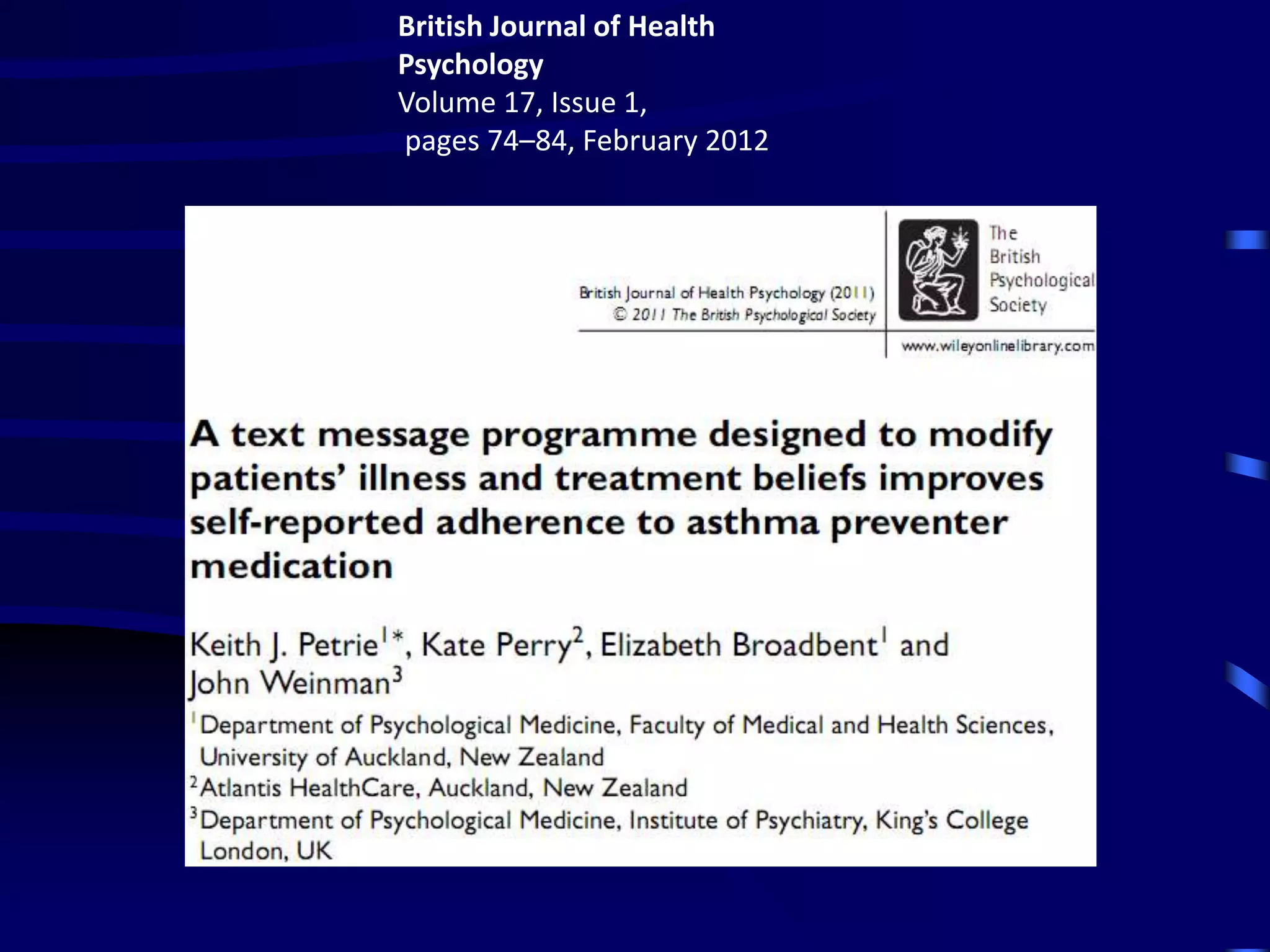
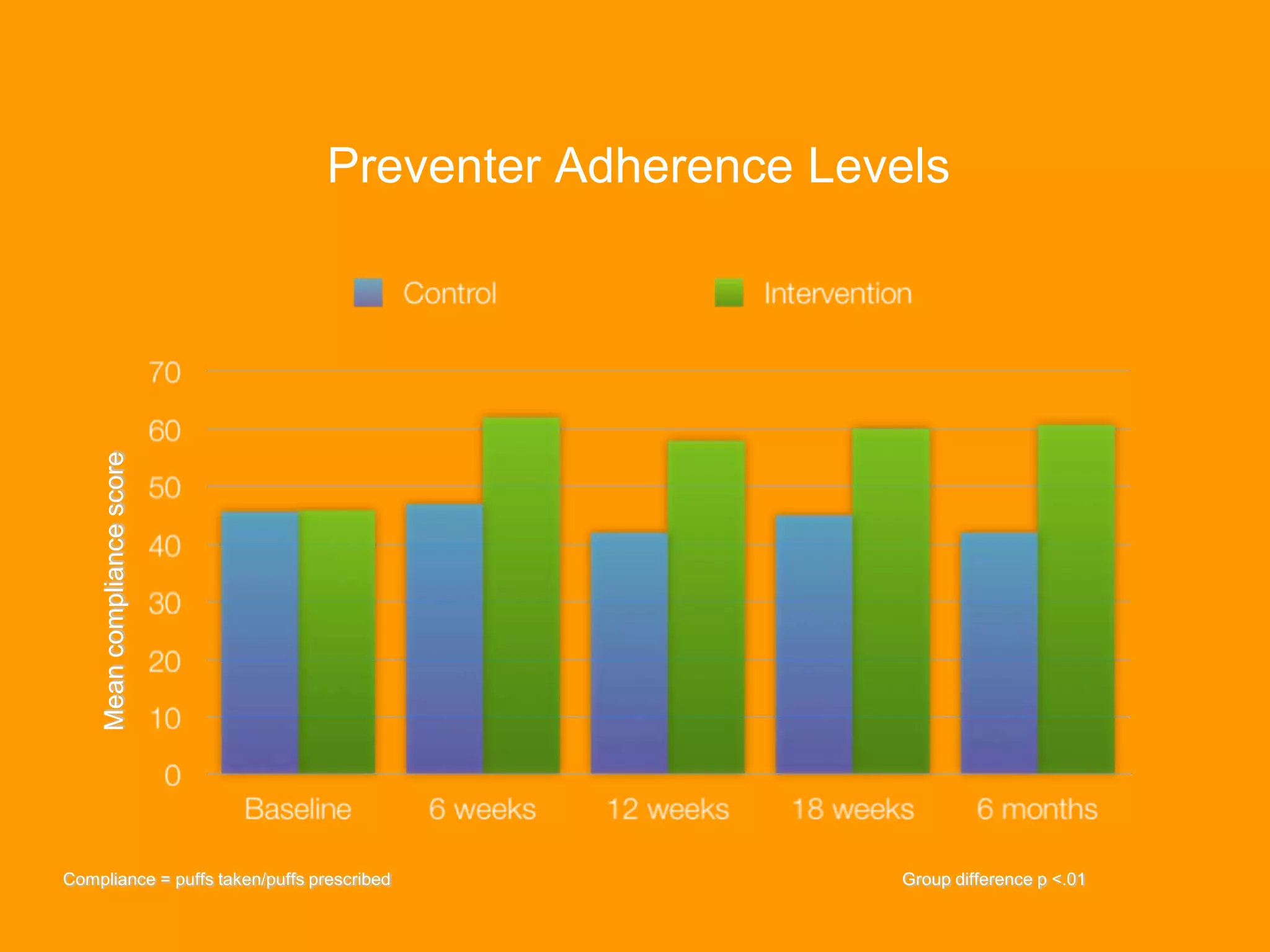
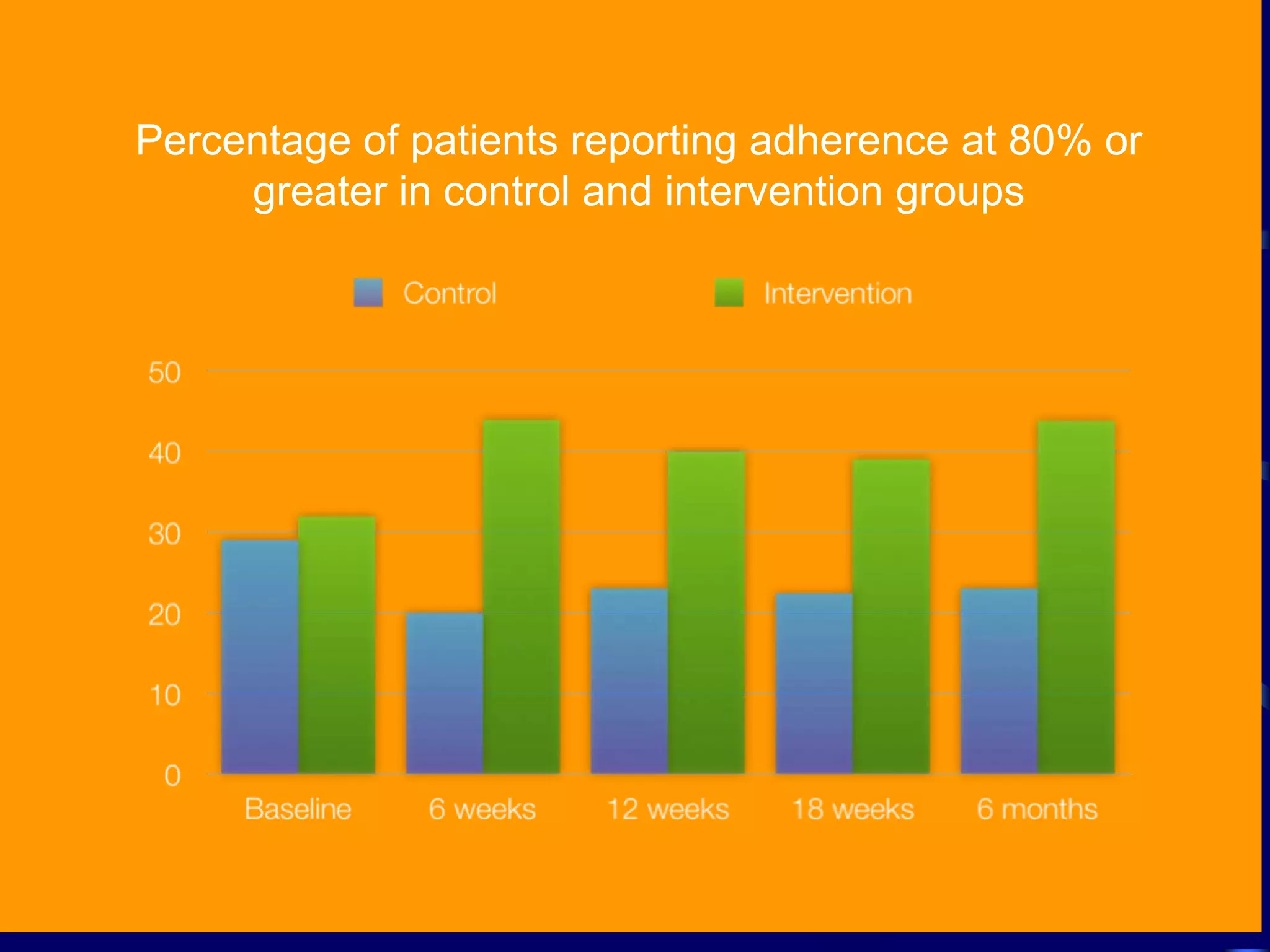
This document discusses patient adherence to medical treatment. It begins by noting estimates that 30-50% of medicines for long-term illnesses are not taken as directed, representing a loss for patients and the healthcare system. Common myths about non-adherence are debunked, and it is argued that patients' perceptions of their illness and prescribed treatment strongly influence adherence. Effective interventions should aim to improve the fit between patients' illness beliefs and treatment recommendations by addressing concerns about necessity and potential adverse effects through clear communication and education.