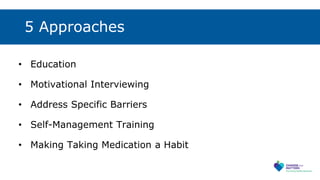
Mr. Avery, a 62-year-old man with diabetes, has poor medication adherence as evidenced by his hemoglobin A1c of 9.0. The provider hopes to address modifiable factors impacting his behavior and establish strategies to improve his medication adherence. Effective approaches include education, motivational interviewing to explore importance and build confidence, addressing specific barriers, training in self-management, and establishing medication-taking as a daily habit. Documentation templates and other resources can help providers structure discussions and monitor adherence over time.