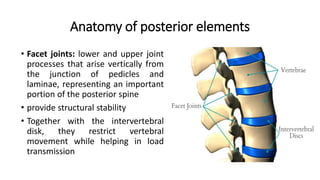
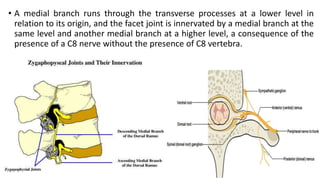
The posterior elements of the spine include the facet joints, ligaments, and processes. Facet joints can develop osteoarthritis due to factors like age, trauma, and disc degeneration. Changes include osteophyte formation, joint space narrowing, and subchondral cysts. Associated conditions are juxtafacet cysts arising from facet joints and ligamentum flavum hypertrophy/cysts. Imaging can identify these degenerative changes and cysts, which may compress nerves and require surgical treatment.