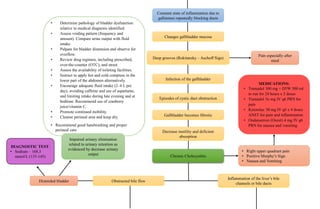
This document discusses the pathophysiology of gallbladder disease in a 29-year-old Asian female with a family history of related conditions. It describes predisposing factors like her age, gender, race, and family history. Precipitating factors included her diet high in cholesterol. The pathophysiology section outlines how gallstones can form and block bile ducts, causing inflammation. Diagnostic tests confirmed choledocholithiasis and cholecystolithiasis. Prescribed medications aim to manage pain, inflammation, and risk of infection post-cholecystectomy surgery. Nursing diagnoses address risks of impaired skin integrity and infection due to the open procedure and T-tube insertion.