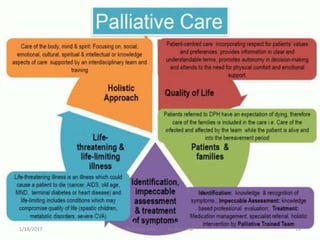
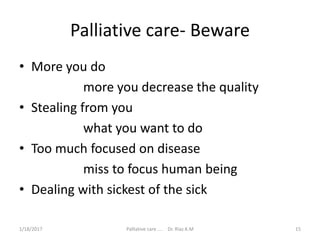
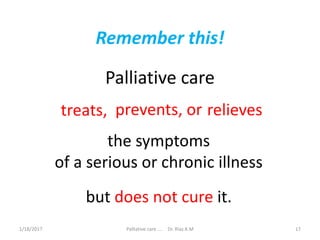
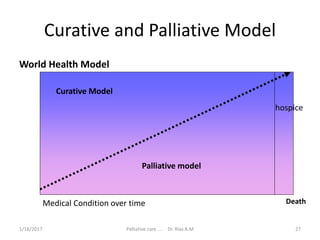
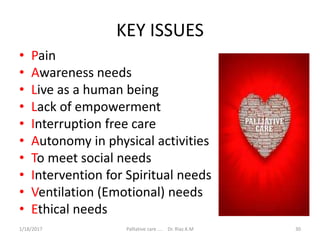
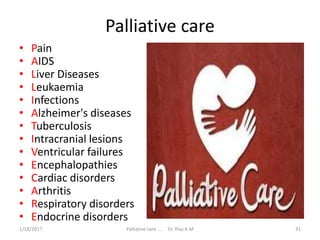
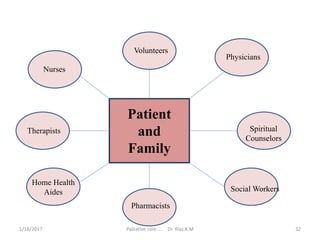
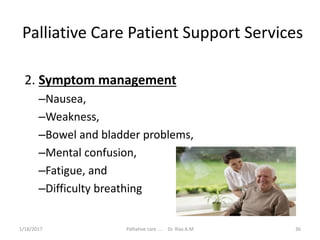
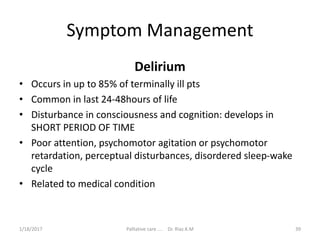
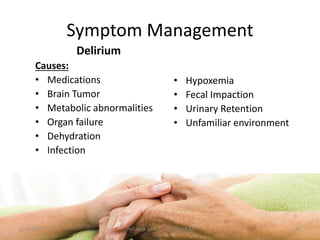
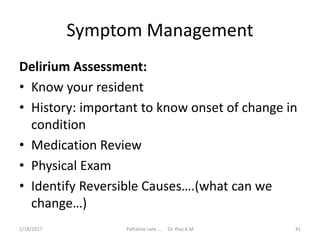
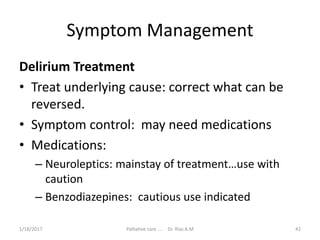
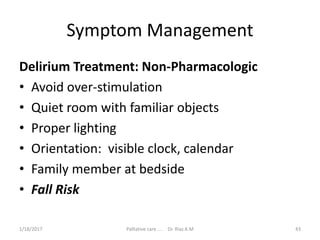
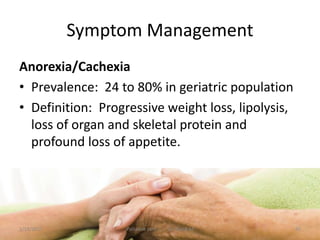
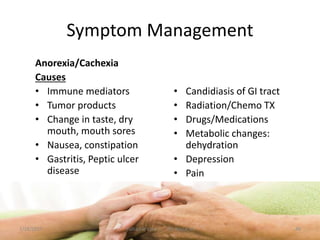
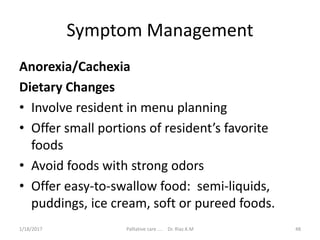
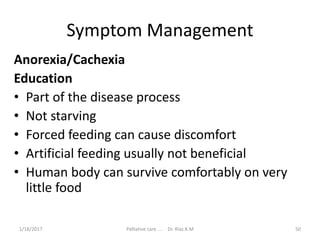
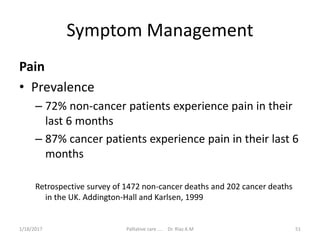
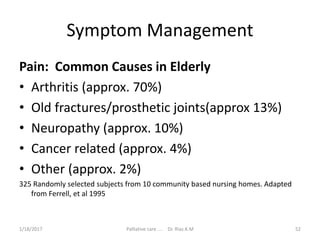
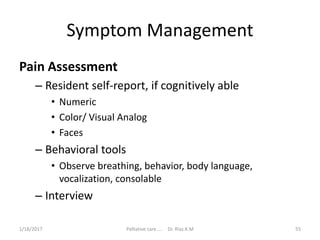
The document describes a story about a tree and a boy who grew up playing by the tree. As the boy grew older, he asked the tree for help building a house, making a boat, and finally for a place to rest. Each time, the tree gave parts of itself to help the boy. In the end, when the old man returned tired, the tree offered its roots for the man to rest on, finding purpose in helping the man even at the end of its life. The document also includes sections about palliative care, focusing on improving quality of life for those with serious illness and their families through managing symptoms.