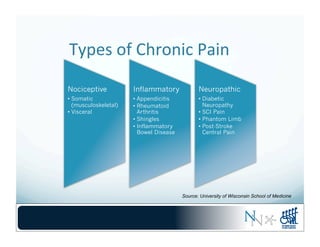
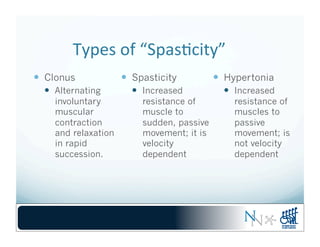
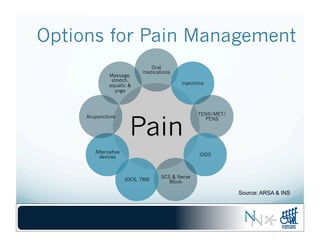
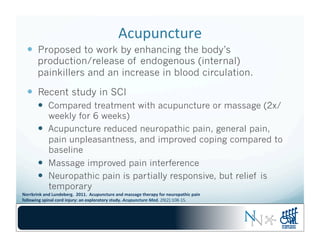
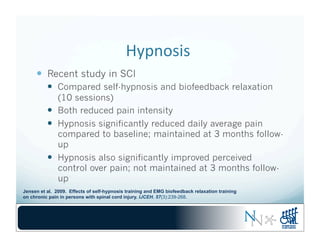
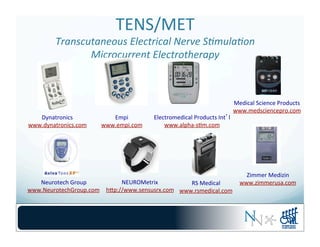
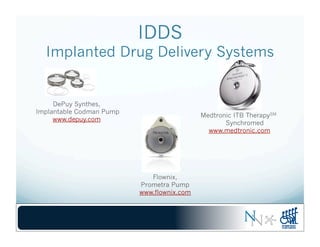
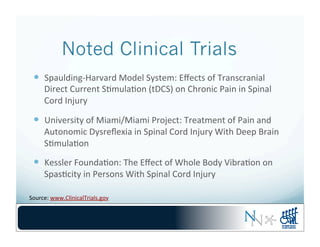
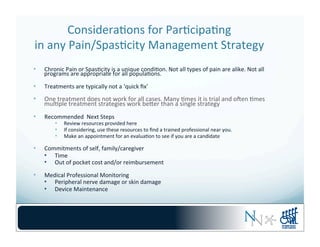
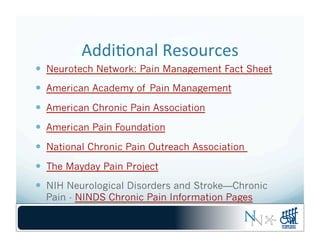
This webinar discusses pain and spasticity management options without medications. It is presented by Kimberly Anderson-Erisman from the University of Miami and Jennifer French from Neurotech Network. The webinar covers types of chronic pain and spasticity, options for pain management including medications, injections, devices, and alternative therapies. Examples of alternative therapies used by people with spinal cord injuries are discussed, such as exercise, stretching, changing position and massage. Technology integration options for pain management including TENS, spinal cord stimulation, transcranial direct current stimulation, and alternative devices are also presented.