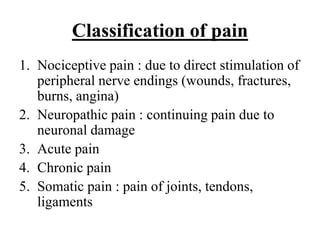
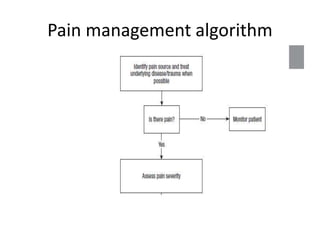
1. The document discusses pain pathways and management. It defines pain and describes the etiology, classification, pathophysiology involving peripheral and central mechanisms, clinical presentation, and treatment including analgesics and non-pharmacological options.
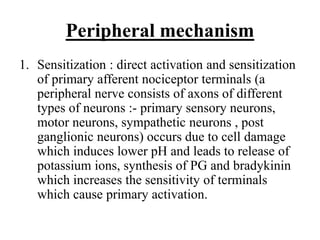
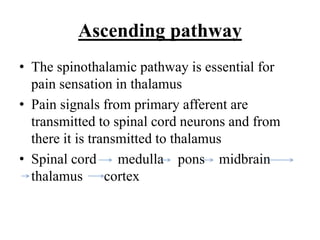
2. The pathophysiology involves sensitization of primary afferent nociceptor terminals and propagation of impulses through the ascending spinothalamic pathway and modulation by descending pathways.
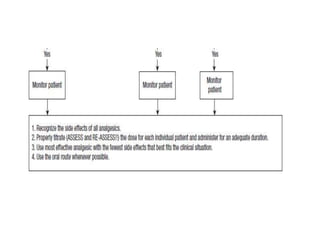
3. Treatment involves a stepwise approach using NSAIDs, opioids, and non-pharmacological alternatives like acupuncture, ayurveda, yoga and meditation.