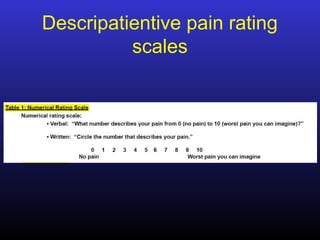
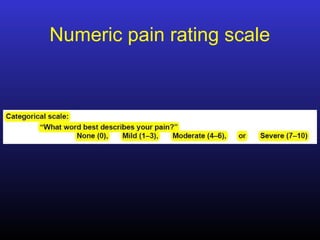
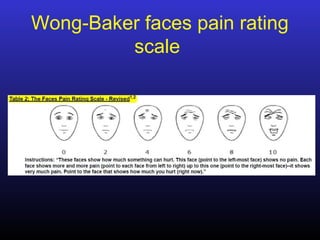
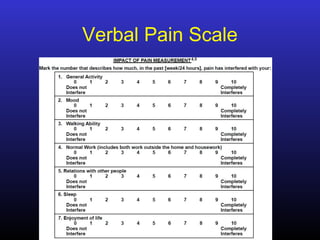
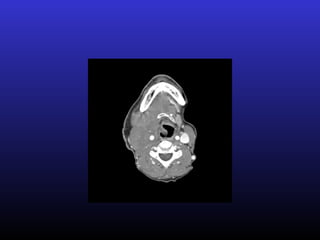
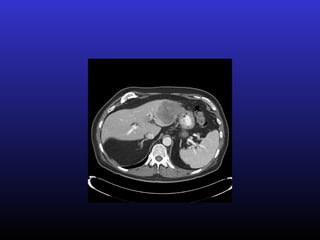
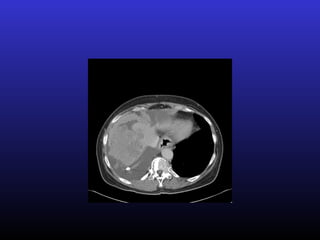
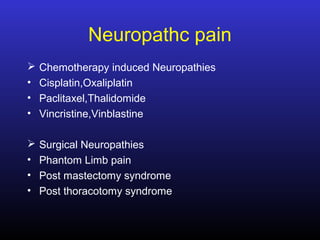
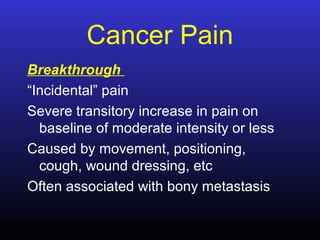
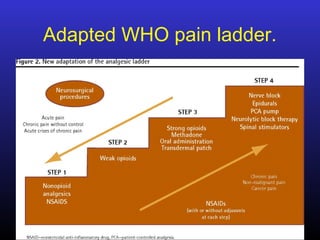
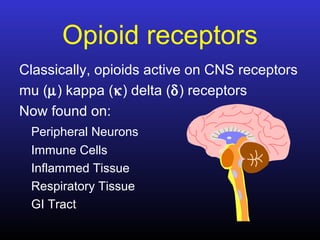
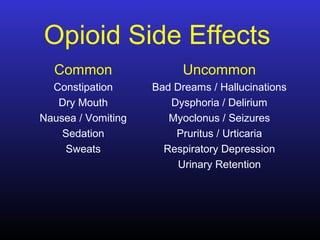
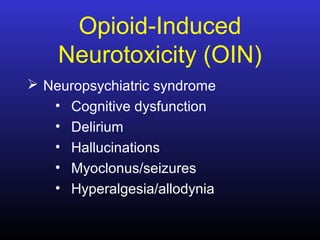
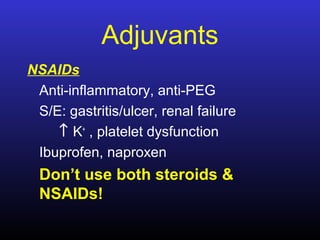
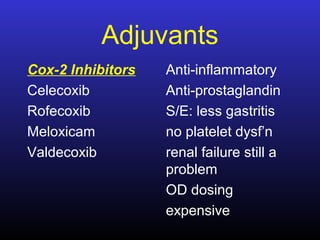
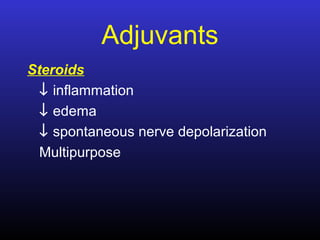
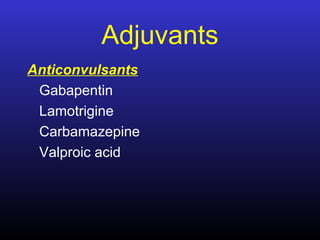
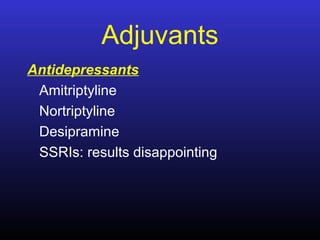
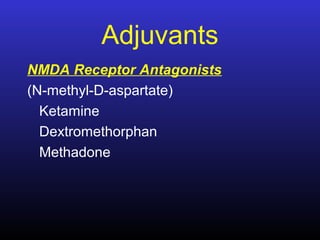
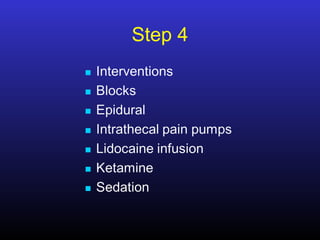
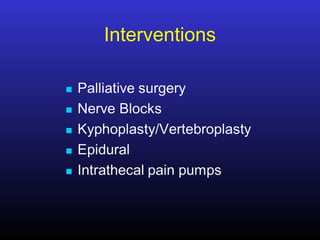
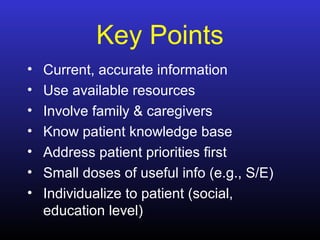
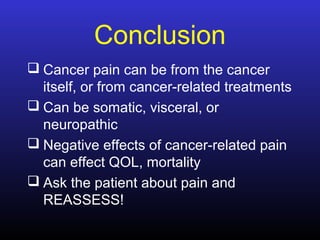
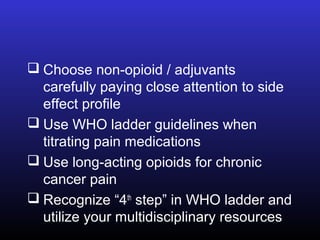
This document discusses pain management in cancer patients. It describes different types of cancer pain such as nociceptive, neuropathic, somatic, visceral, and bony pain. It also discusses various pain rating scales. Treatment options covered include opioids, NSAIDs, steroids, bisphosphonates, radiation, surgery, and adjuvants like anticonvulsants and antidepressants. Non-pharmacological options like acupuncture and alternative therapies are also mentioned. The conclusion emphasizes the importance of comprehensive cancer pain assessment and management using a multidisciplinary approach.