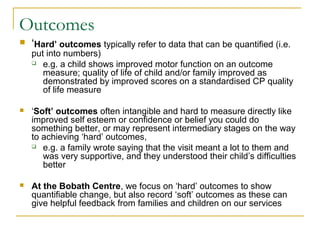
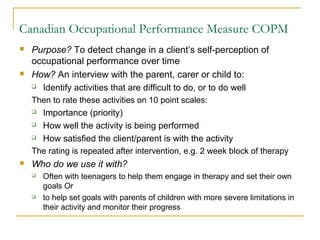
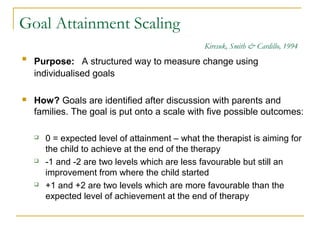
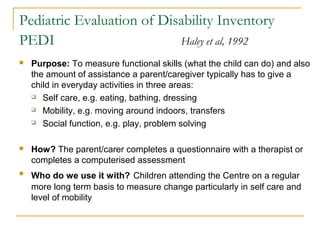
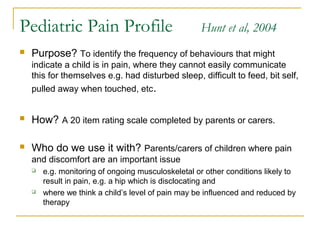
The document discusses outcome measures used at the Bobath Centre to measure changes in patients receiving therapy. A variety of outcome measures are used to quantify changes in motor function, quality of life, pain levels, and functional abilities. Outcome measures are administered before and after therapy to track improvements in areas like mobility, self-care, social skills, and spinal alignment. Both standardized tests and individualized goal attainment scales are utilized to systematically evaluate the effects of treatment.