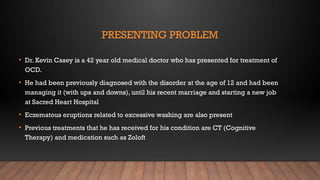
The document discusses Obsessive Compulsive Disorder (OCD), detailing its characteristics, prevalence, diagnostic criteria, and treatment options, through the case study of Dr. Kevin Casey. It highlights how OCD manifests in behaviors and thoughts, alongside the history of its classification in mental health diagnostics. Treatment strategies include a combination of pharmacotherapy and psychotherapy, focusing on Cognitive Behavioral Therapy and Exposure and Response Prevention.




























![REFERENCES
• American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5.
Washington, D.C: American Psychiatric Association.
• Anxietybc.com. (2015).What Is Obsessive-Compulsive Disorder? | Anxiety BC. [online] Available at:
http://www.anxietybc.com/resources/ocd.php
• Foa, E.B., (2010). Cognitive behavioral therapy of obsessive-compulsive disorder. Dialougues Clinical
Neuroscience, 12, 199-207
• Garcia AM Sapyta JJ Moore PS Freeman JB et al (2010). Predictors and moderators of treatment outcome in the
Pediatric Obsessive Compulsive Treatment Study (POTS I). Journal of the American Academy of Child and
Adolescent Psychiatry 49, 1024–1033. https://doi.org/10.1016/j.jaac.2010.06.013
• Helpguide.org. (2015). Obsessive-Compulsive Disorder (OCD): Symptoms, Behavior, and Treatment. [online]
Available at: http://www.helpguide.org/articles/anxiety/obssessive-compulsive-disorder-ocd.htm
• Huffman, K. and Dowdell, K. (2015). Psychology In Action. 11th ed. Hoboken, NJ:Wiley Custom Learning Solutions,
pp.462, 481-484.](https://image.slidesharecdn.com/ocd-240926033630-0d8a5109/85/Obsessive-Compulsive-Disorder-OCD-Presentation-31-320.jpg)
![REFERENCES
• Mayoclinic.org. (2016). Obsessive-compulsive disorder (OCD) Tests and diagnosis - Mayo Clinic. [online] Available at:
http://www.mayoclinic.org/diseases-conditions/ocd/basics/tests-diagnosis/con-20027827
• Nichols, H. (2014).What is obsessive-compulsive disorder (OCD)? What causes obsessive-compulsive behavior?. [online]
Medical News Today. Available at: http://www.medicalnewstoday.com/articles/178508.php
• Robinson, L., Smith, M. and Segal, J. (2015). Obsessive-Compulsive Disorder (OCD): Symptoms, Behavior, and Treatment.
[online] Helpguide.org. Available at: http://www.helpguide.org/articles/anxiety/obssessive-compulsive-disorder- ocd.htm
• Thomsen, P.,Torp, N., Dahl, K., Christensen, K., Englyst, I., Melin, K., Nissen, J., Hybel, K.,Valderhaug, R.,Weidle, B.,
Skarphedinsson, G., Bahr, P. and Ivarsson,T. (2013).The Nordic long-term OCD treatment study (NordLOTS): rationale, design, and
methods. Child and Adolescent Psychiatry and Mental Health, [online] 7(1), p.41. Available at: http://dx.doi.org/10.1186/1753-
2000-7-41
• Weidle, B., Ivarsson,T.,Thomsen, P., Lydersen, S. and Jozefiak,T. (2014). Quality of life in children with OCD before and after
treatment. European Child & Adolescent Psychiatry, [online] 24(9), pp.1061-1074. Available at:
http://dx.doi.org/10.1007/s00787-014-0659-z
• www.nami.org. (2015).The Invisible Disease: An OCD Account. [online] Available at: http://www.nami.org/Personal- Stories/The-
Invisible-Disease-An-OCD-](https://image.slidesharecdn.com/ocd-240926033630-0d8a5109/85/Obsessive-Compulsive-Disorder-OCD-Presentation-32-320.jpg)