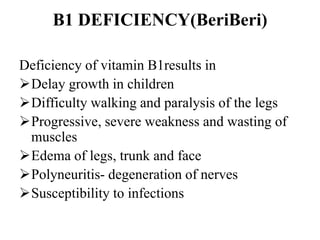
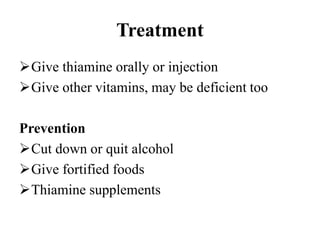
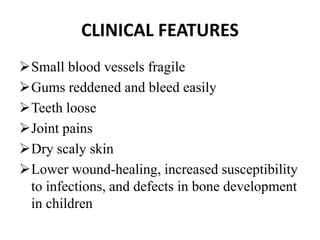
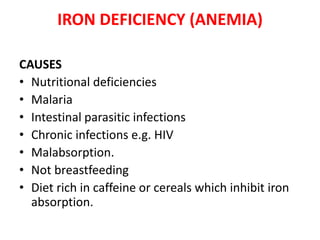
The document discusses nutritional disorders, particularly malnutrition and its forms, such as protein-energy malnutrition (PEM), rickets, and various vitamin deficiencies, detailing their causes, symptoms, and management strategies. It emphasizes the importance of education, socioeconomic factors, and healthcare interventions in addressing and preventing these disorders. Specific nutrient deficiencies like vitamin A, D, iodine, and zinc are also highlighted, alongside treatment options and preventive measures to improve overall nutritional health.