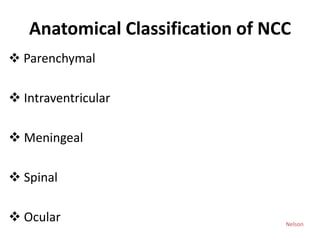
The document provides a comprehensive overview of neurocysticercosis (NCC), including its causative agent Taenia solium, clinical features, and anatomical classifications. It discusses various stages of cyst formation, diagnostic methods, management strategies, and differential diagnoses to distinguish NCC from other conditions. Additionally, it emphasizes the importance of prevention through proper hygiene and food handling practices.