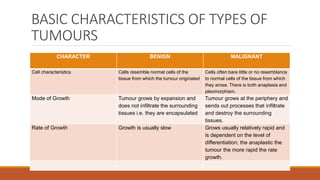
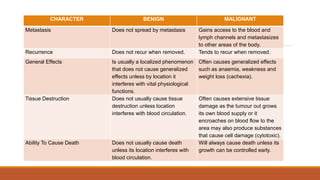
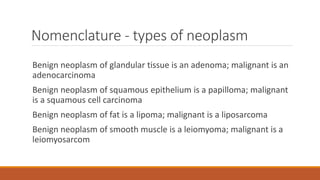
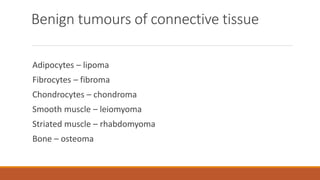
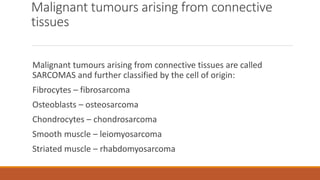
Neoplasms refer to abnormal tumour growth. They can be benign or malignant. The key characteristics that distinguish malignant neoplasms from benign ones are their ability to invade surrounding tissues and metastasize to other parts of the body. Malignant neoplasms also have less differentiated cells, grow more rapidly, and will ultimately cause death if not treated. Accurately staging cancers by describing tumour size, lymph node involvement, and metastasis is important for determining prognosis and selecting appropriate treatment options.