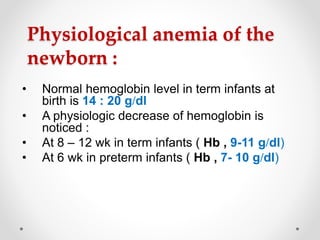
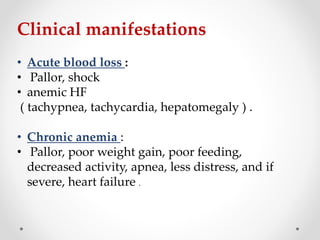
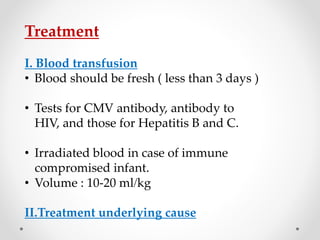
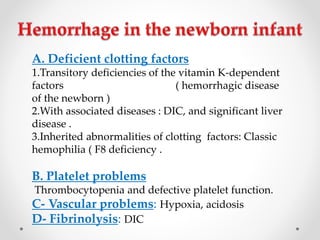
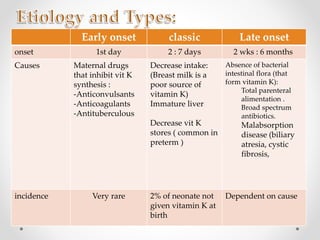
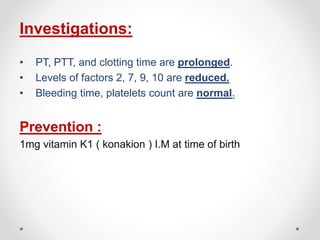
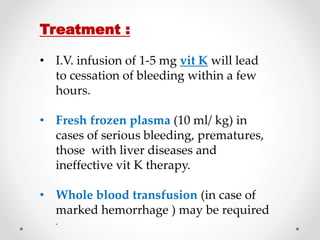
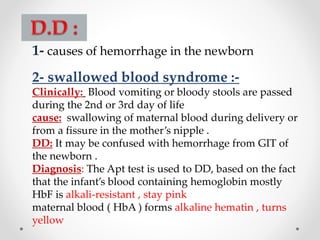
This document discusses neonatal hematological disorders, including physiological anemia of the newborn, pathological anemia, and hemorrhagic disease of the newborn. Physiological anemia occurs as hemoglobin levels normally decrease after birth. Pathological anemias can result from blood loss, hemolysis, or diminished red blood cell production. Hemorrhagic disease of the newborn is caused by vitamin K deficiency and can cause bleeding at injection sites, in the GI tract, or intracranially. Treatment involves vitamin K supplementation to prevent hemorrhagic disease, and blood transfusions to treat blood loss or low hemoglobin levels.