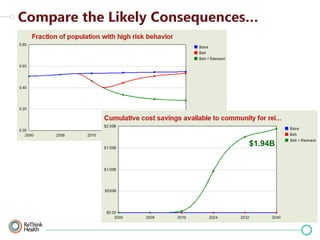
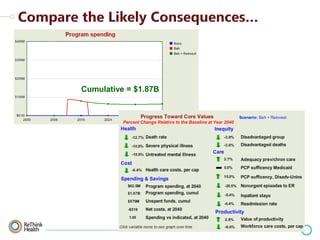
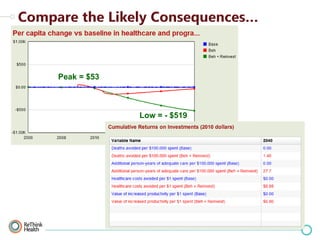
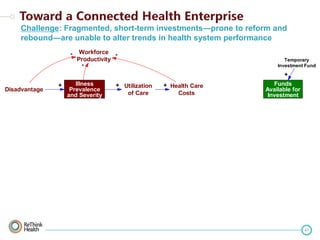
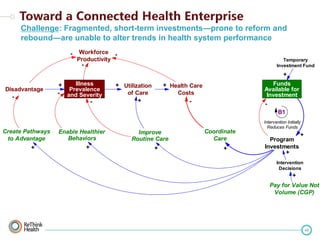
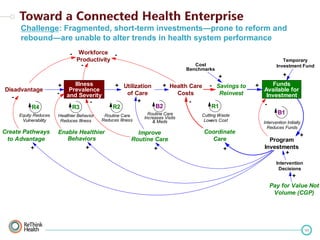
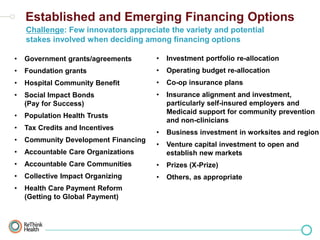
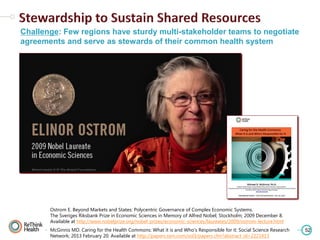
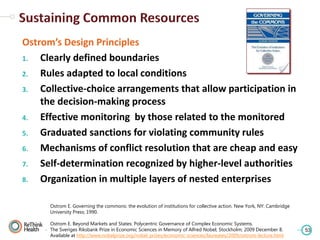
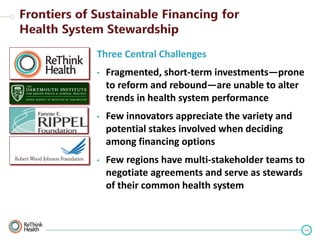
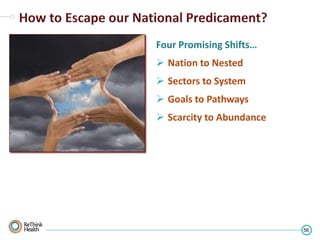
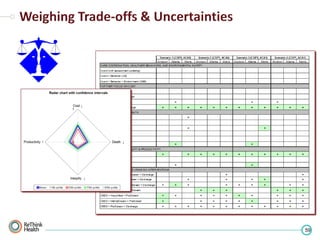
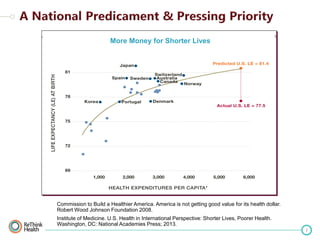
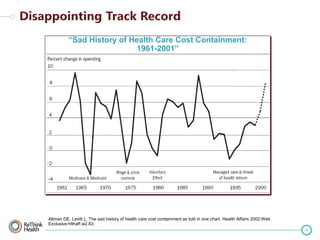
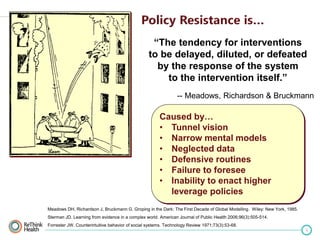
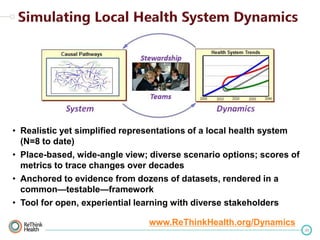
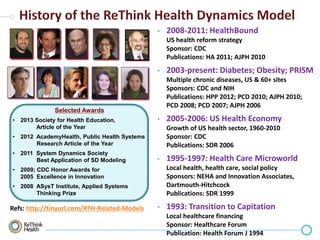
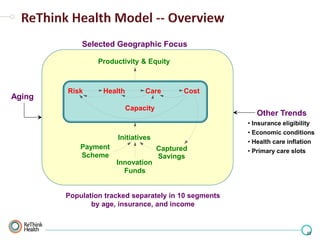
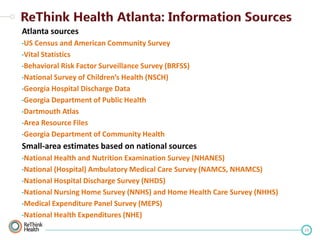
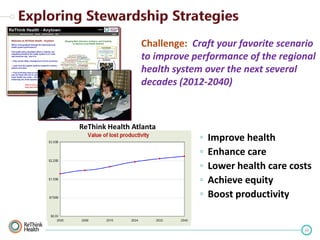
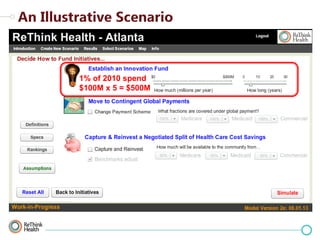
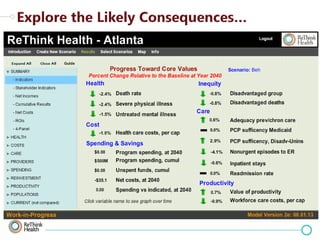
The document discusses the inefficiencies and systemic issues within the U.S. health care system, highlighting that increased spending has not correlated with better health outcomes. It emphasizes the need for innovative strategies and collaborative approaches to create sustainable improvements in health care performance. Key challenges include fragmented investments, lack of multi-stakeholder engagement, and the necessity for a significant shift in how health systems are financed and managed.



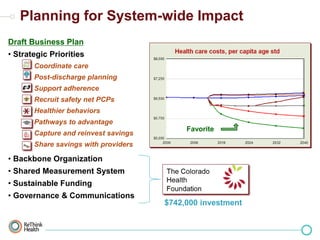

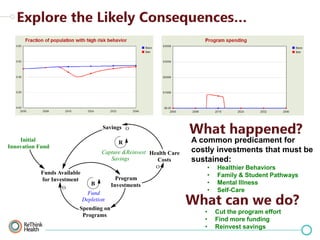
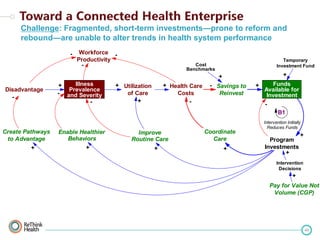
![“Savings generated from improved
[clinical] practice and performance could
also be reinvested in the community,
creating a reinforcing loop.”
-- Sanne Magnan, Elliott Fisher, David Kindig,
George Isham, Doug Wood, Mark Eustis,
Carol Backstrom, Scott Leitz
Magnan S, Fisher E, Kindig D, et al. Achieving Accountability for Health and
Health Care Minneapolis, MN; 2012 July 10. Available at
http://tinyurl.com/icsi-AHC](https://image.slidesharecdn.com/milsteingr-beyondreformandreboundv6-131107125941-phpapp01/85/Dr-Bobby-Milstein-Beyond-Reform-and-Rebound-36-320.jpg)