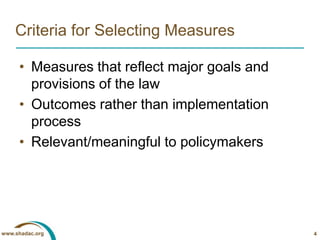
This presentation discusses metrics and data sources for measuring the impact of state-level health reform. It identifies priority measures for health insurance coverage, affordability and comprehensiveness of coverage, and access to care. Existing data sources like surveys are identified, but there are also gaps, particularly for private insurance premiums and nongroup coverage comprehensiveness. Challenges in using population surveys across states are discussed. Planning is needed to uniformly collect high-priority data not currently available to accurately measure state health reform impacts.