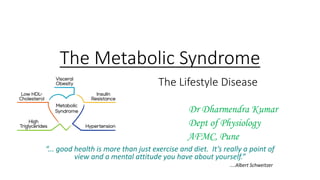
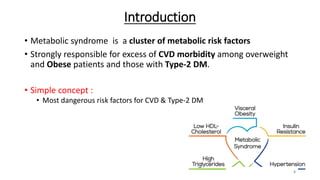
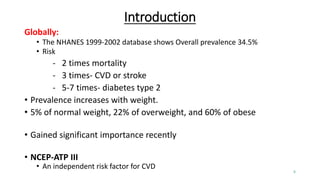
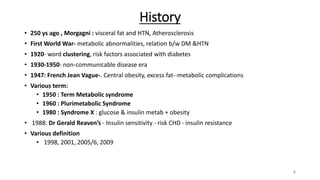
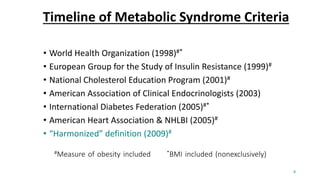
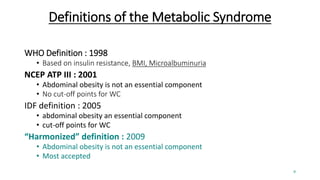
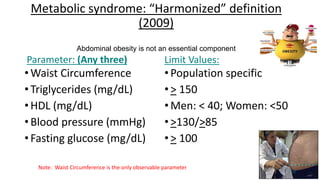
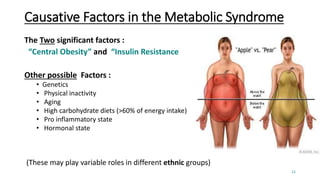
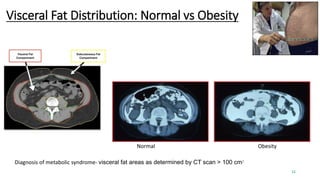
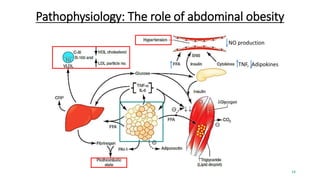
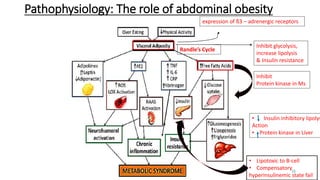
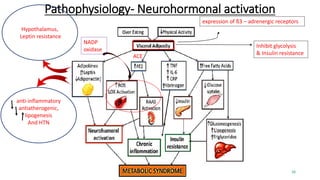
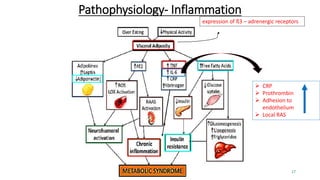
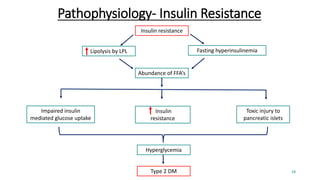
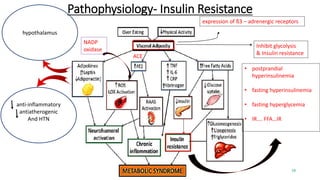
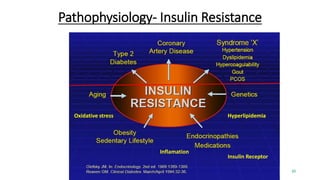
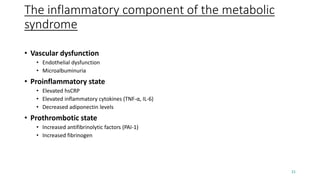
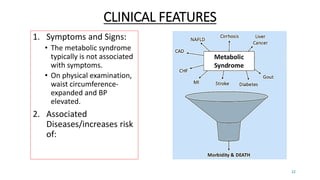
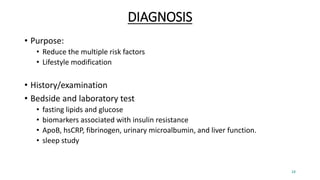
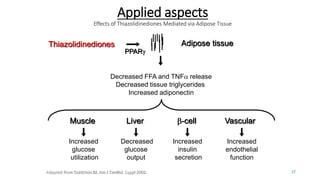
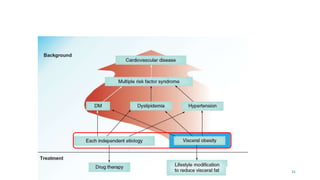
Metabolic syndrome, also known as insulin resistance syndrome, is a cluster of metabolic risk factors that significantly increases cardiovascular disease (CVD) and type-2 diabetes risk, particularly in overweight and obese individuals. Despite variations in diagnostic criteria, key components include central obesity and insulin resistance, with lifestyle modification being crucial for prevention and management. Recent advances in therapies and a growing emphasis on understanding the syndrome highlight its global epidemic status and the need for proactive health evaluations.