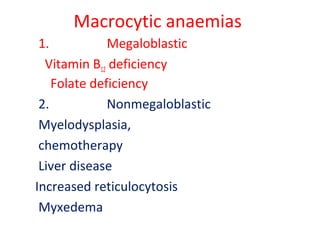
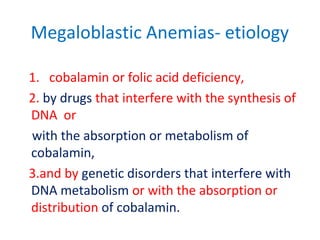
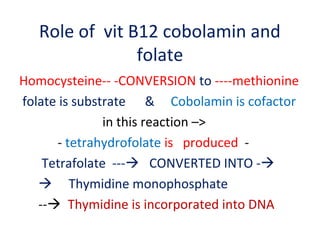
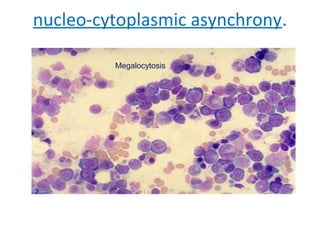
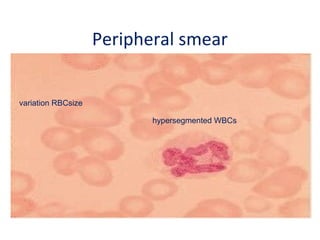
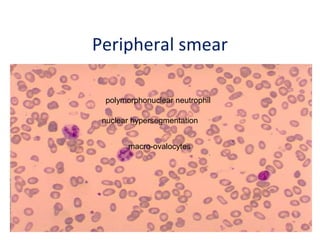
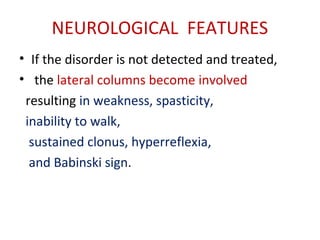
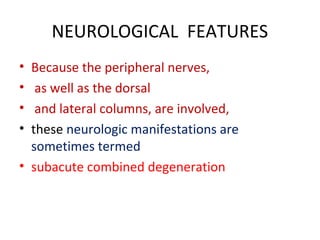
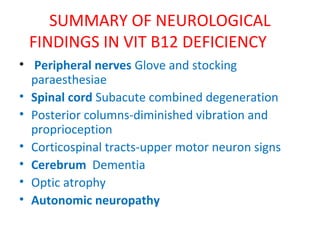
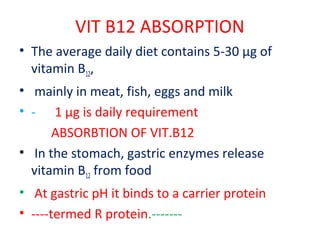
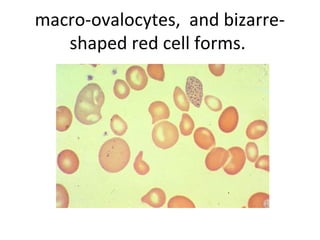
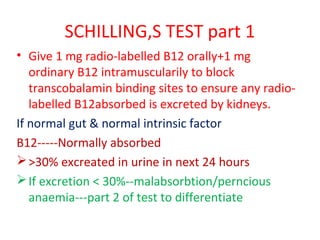
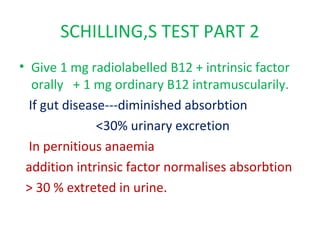
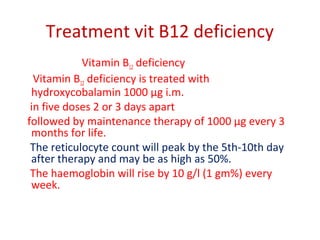
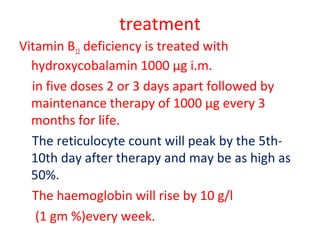
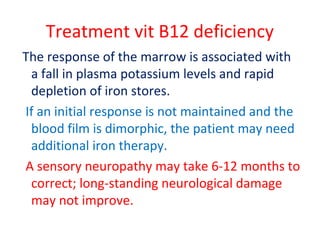
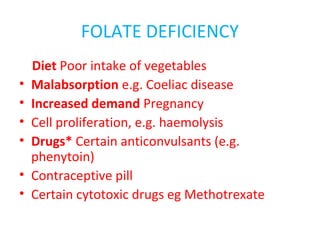
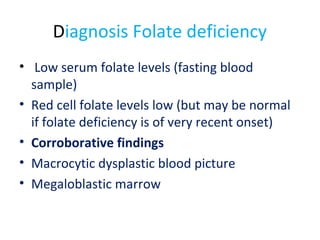
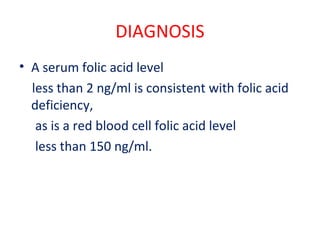
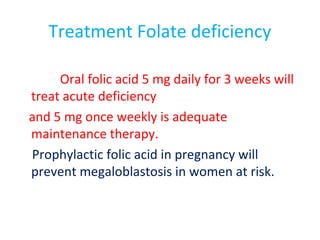
Vitamin B12 and folate deficiencies can cause megaloblastic anemia due to impaired DNA synthesis. Vitamin B12 deficiency specifically can also cause neurological manifestations like peripheral neuropathy. Diagnosis involves blood tests showing macrocytic anemia and low vitamin levels. Treatment is with high dose vitamin B12 injections initially then maintenance doses to correct the deficiency. Folate deficiency has similar blood features but no neurological involvement, and is treated with oral folic acid supplementation.