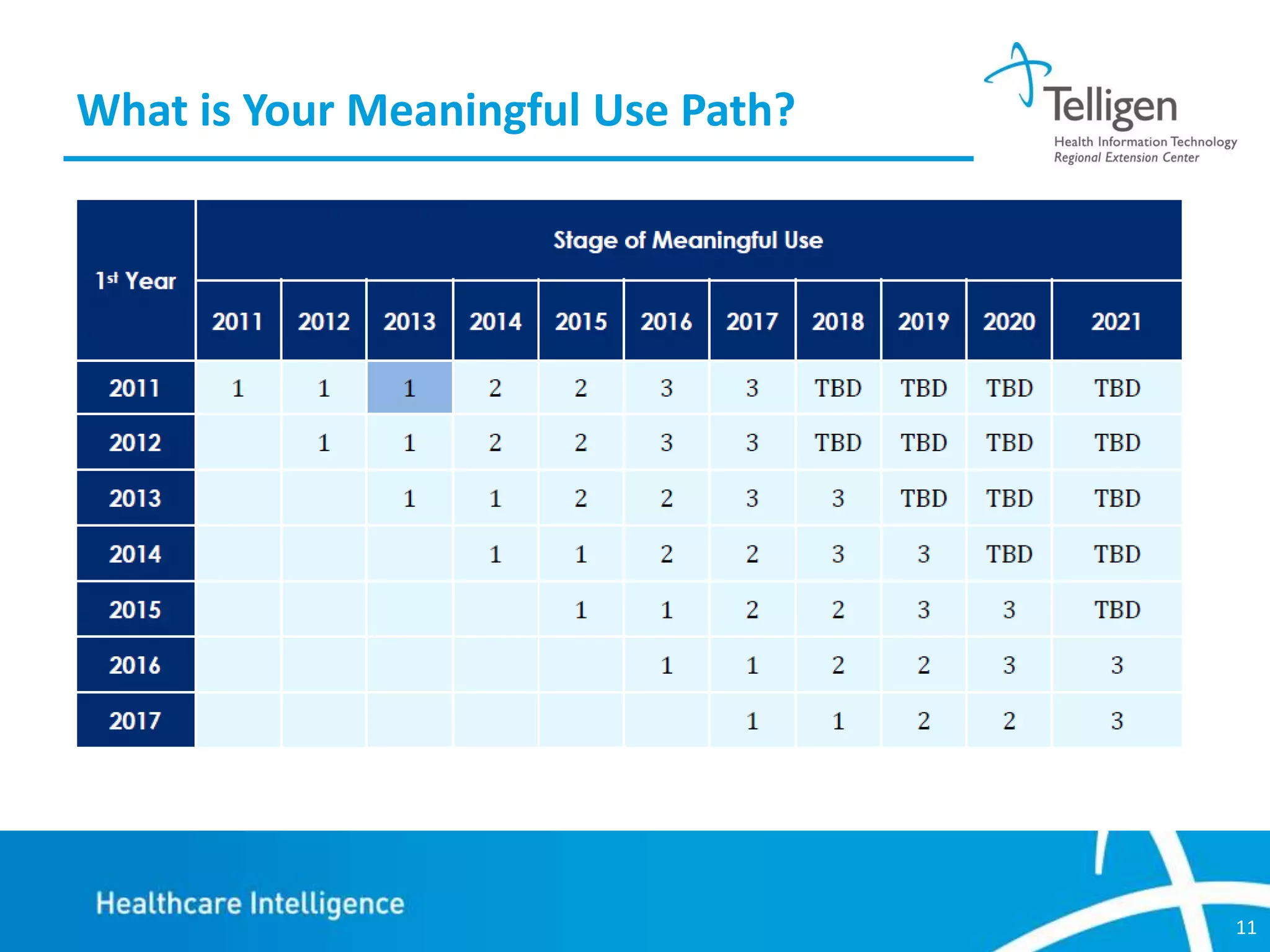
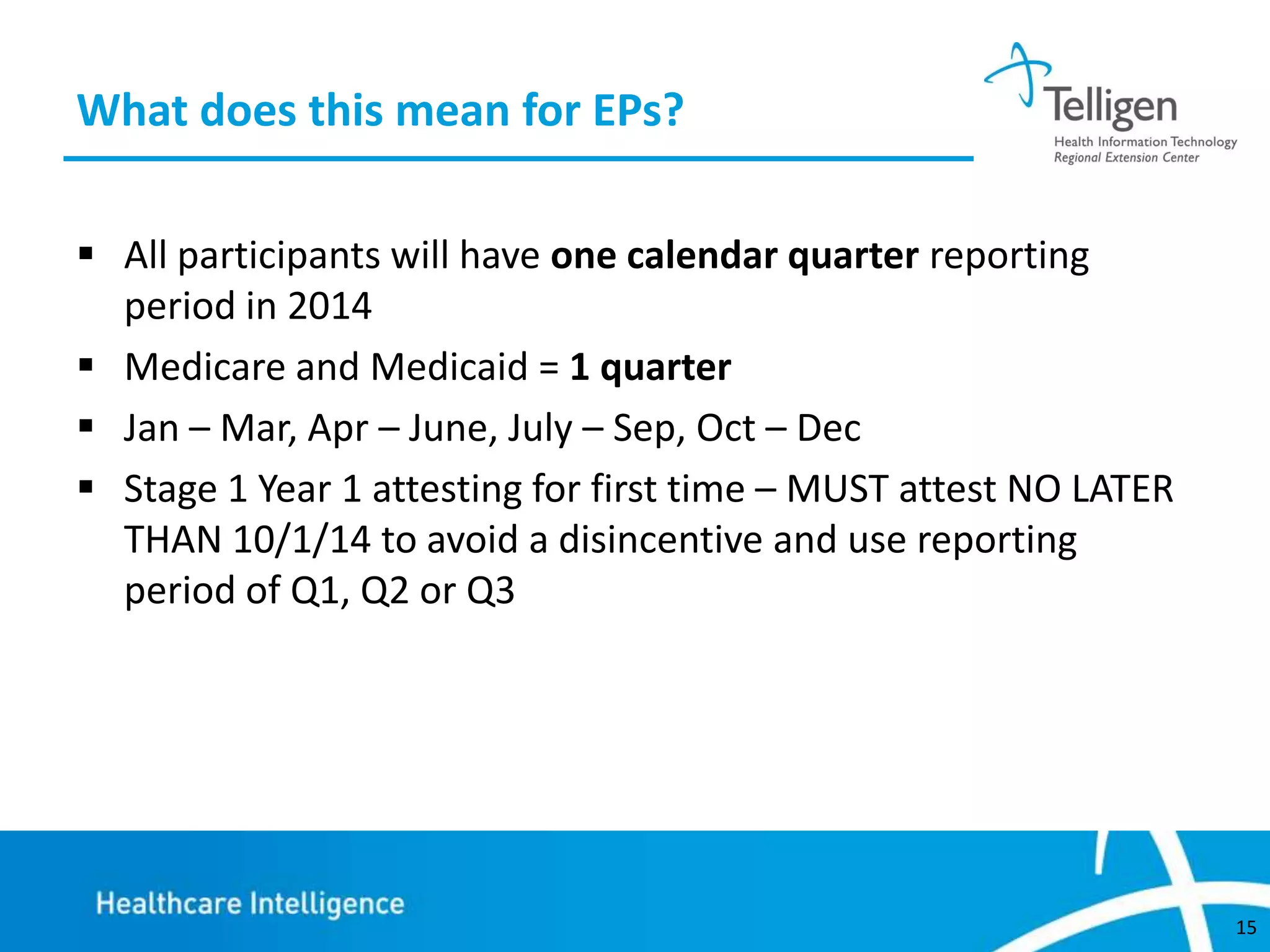
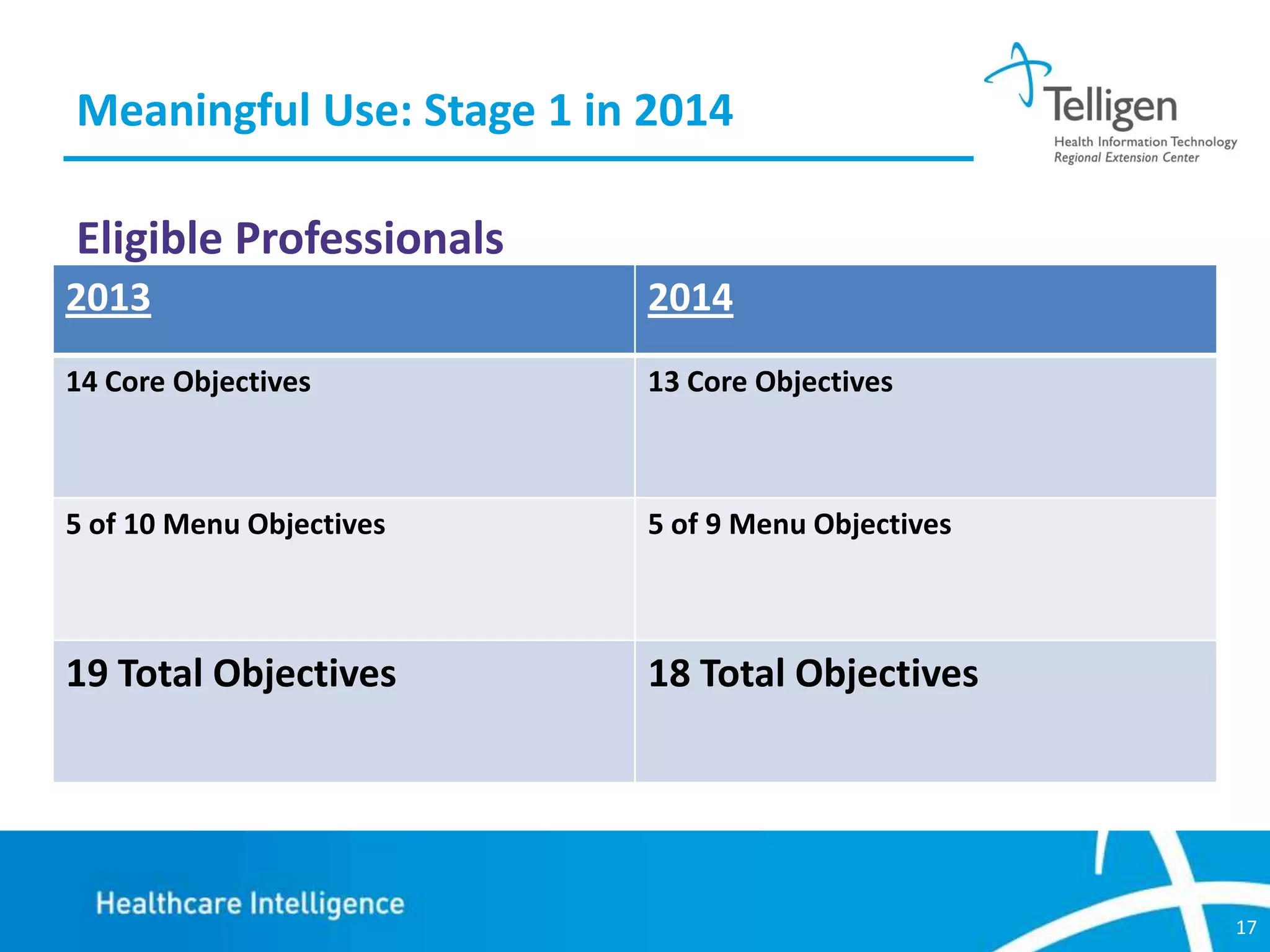
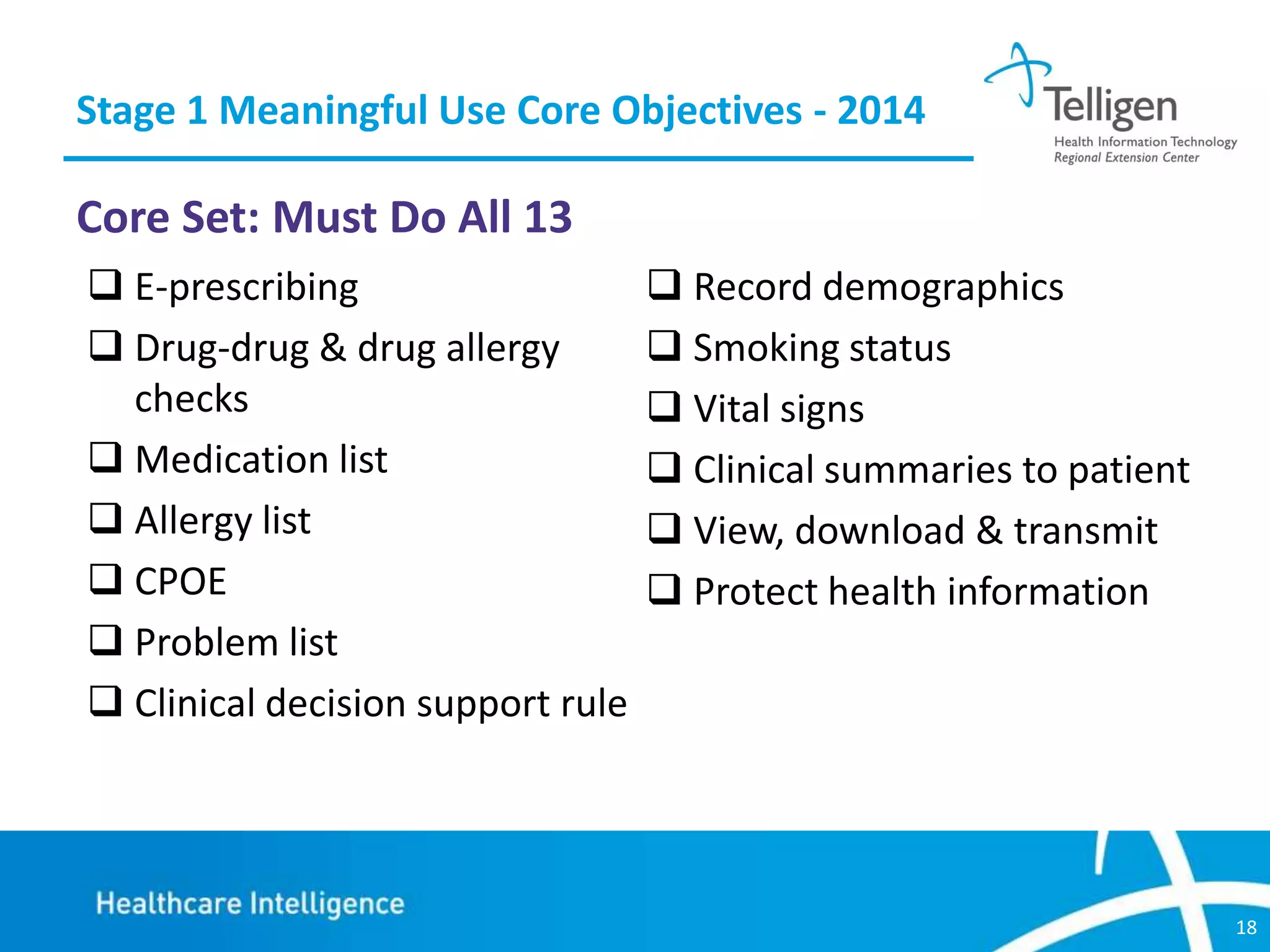
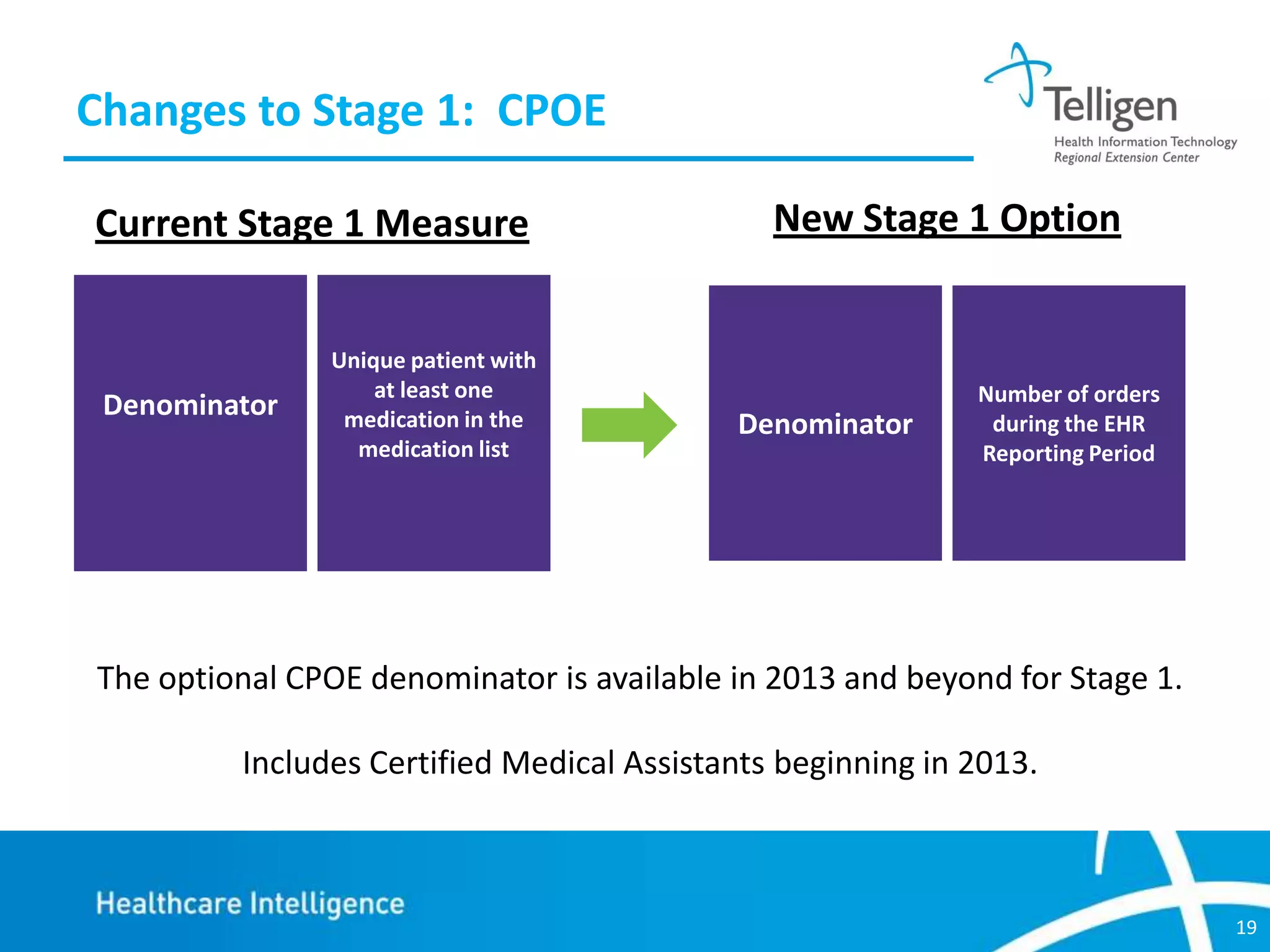
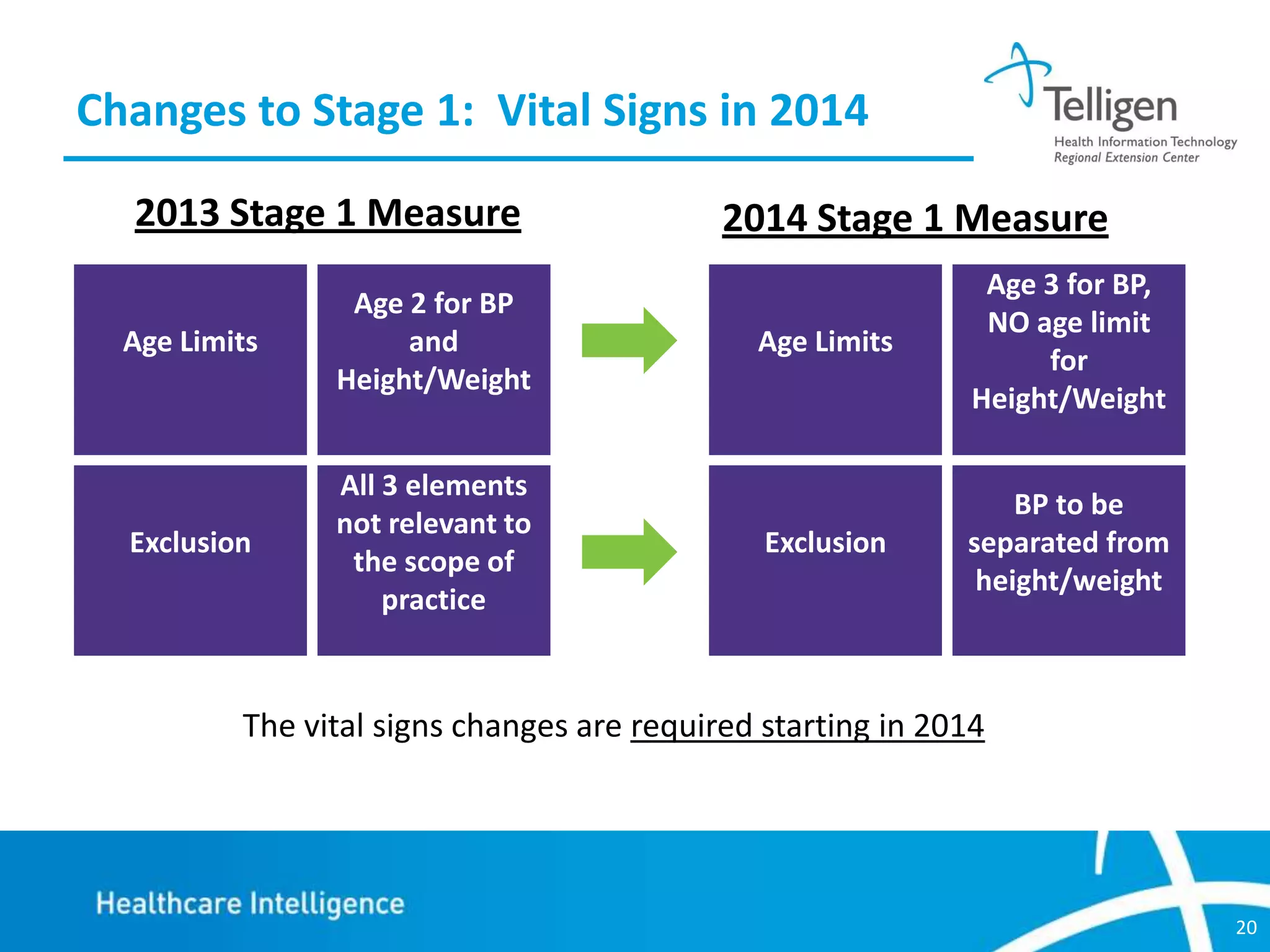
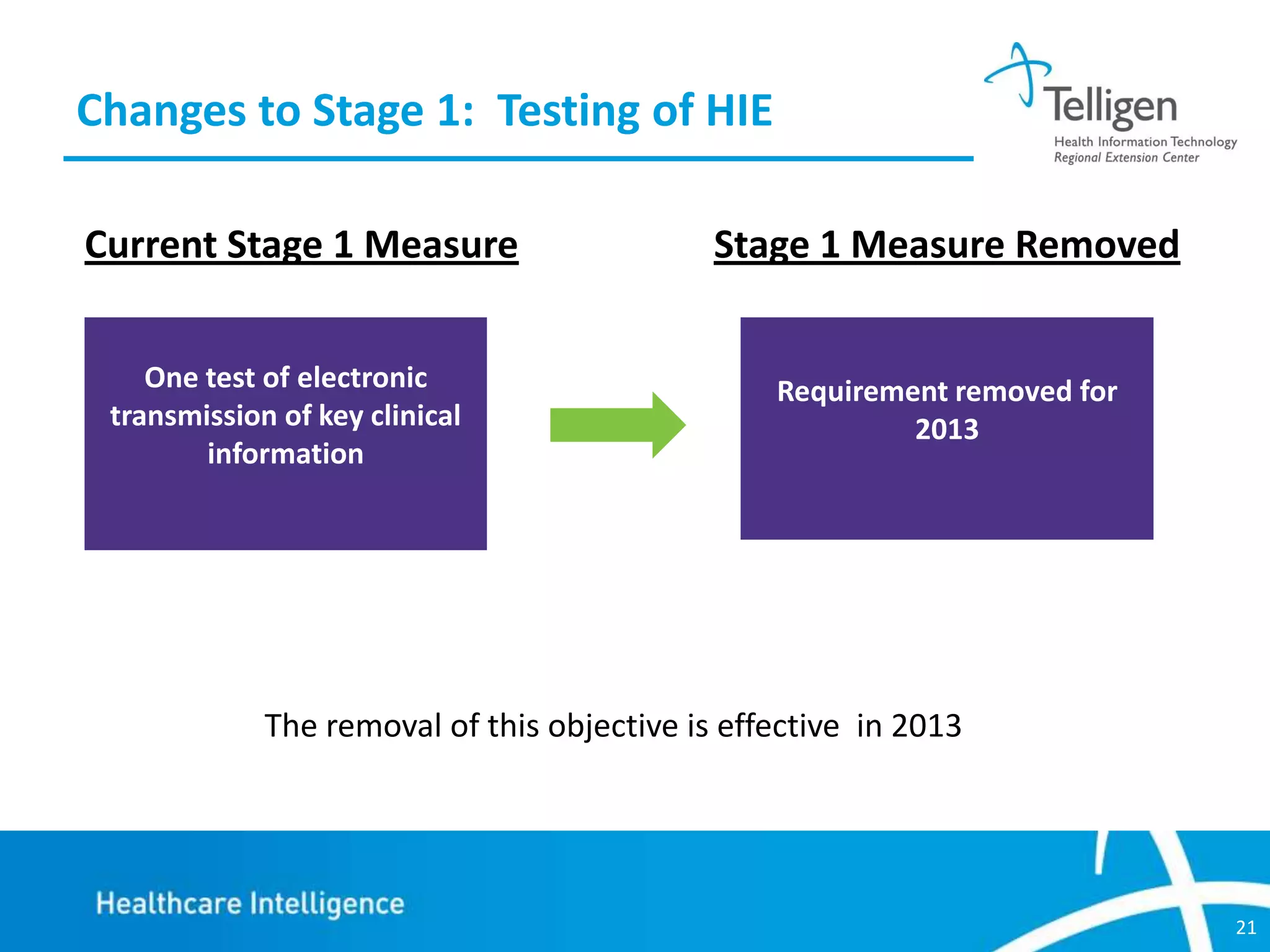
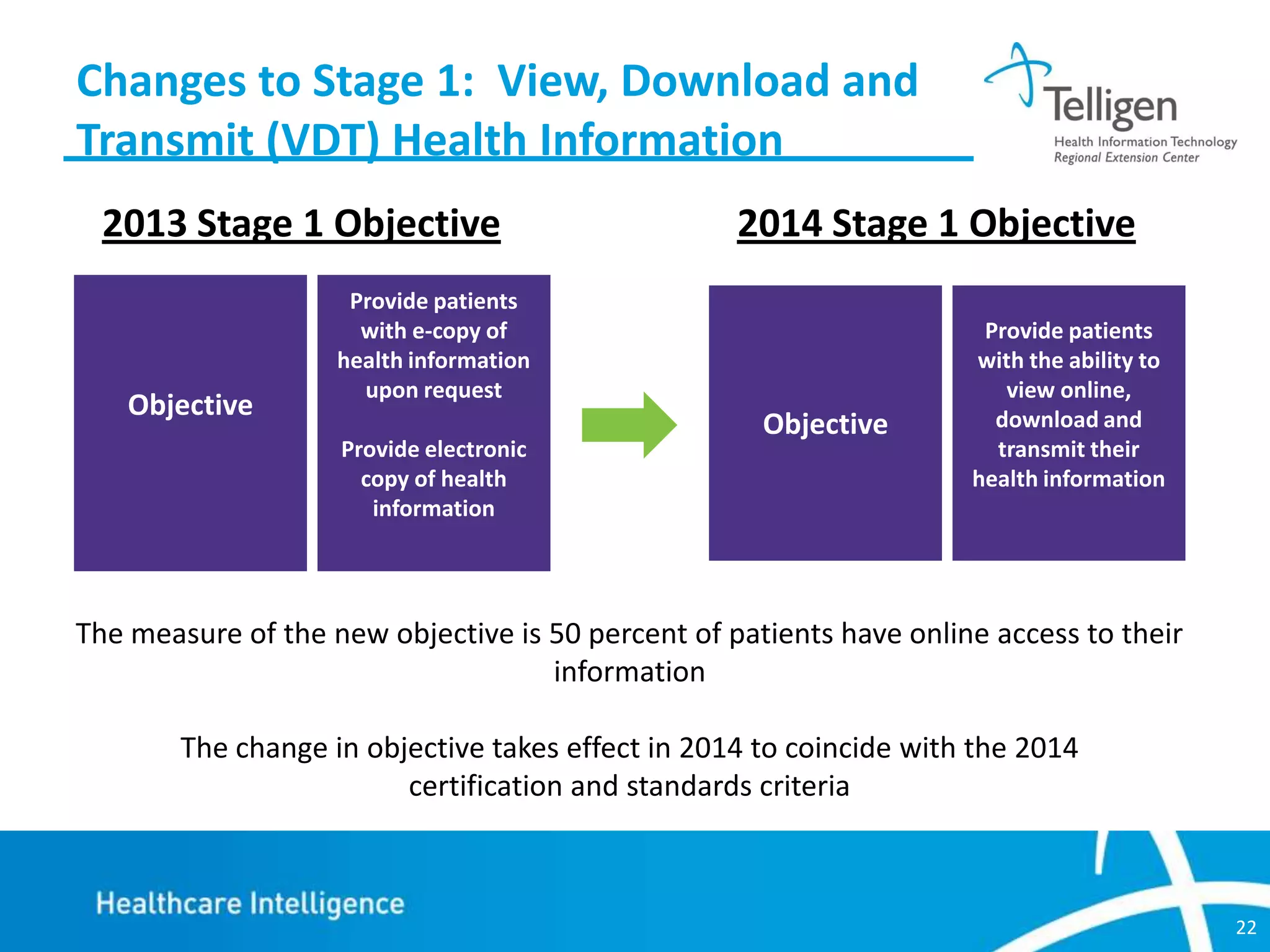
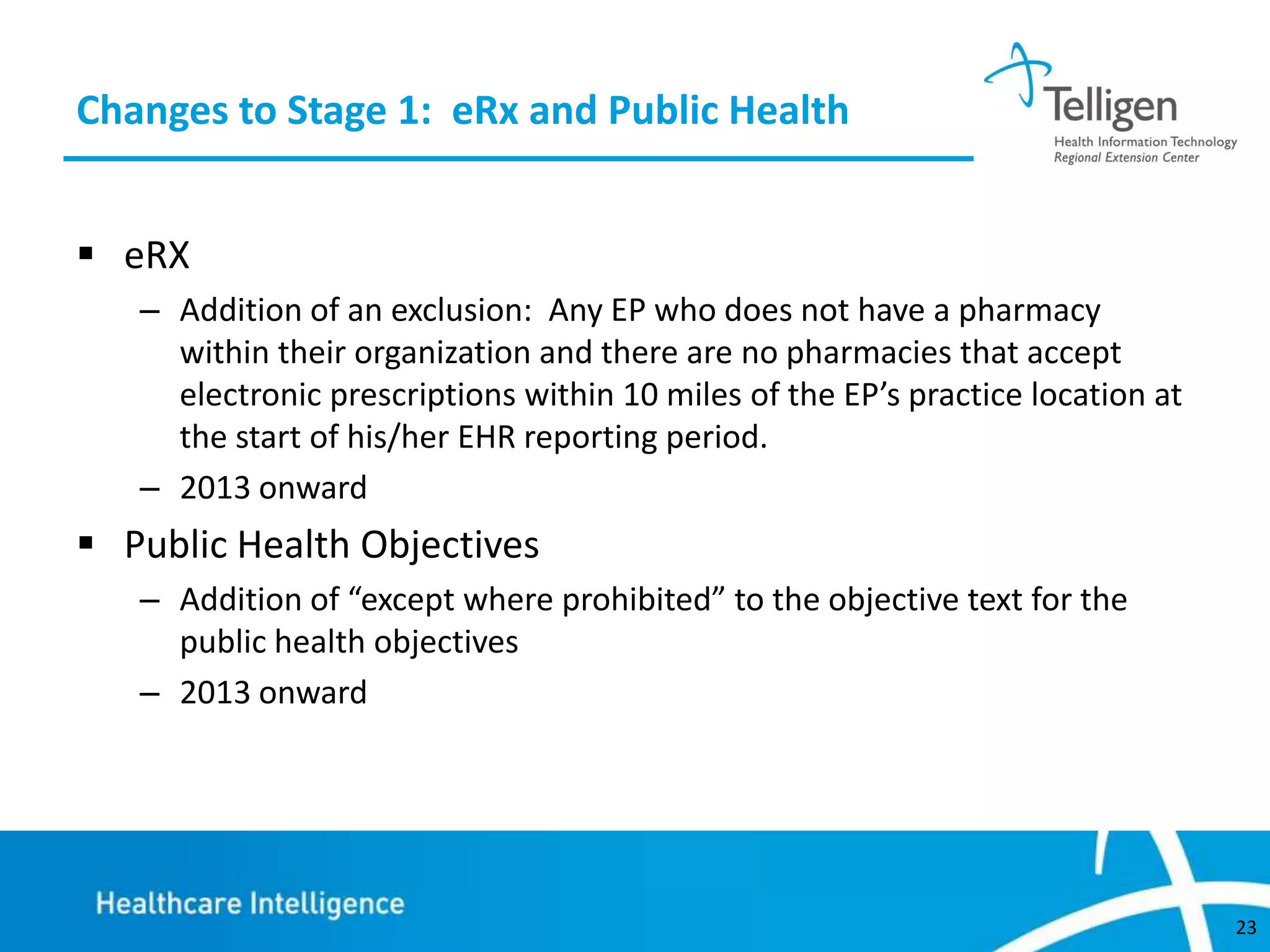
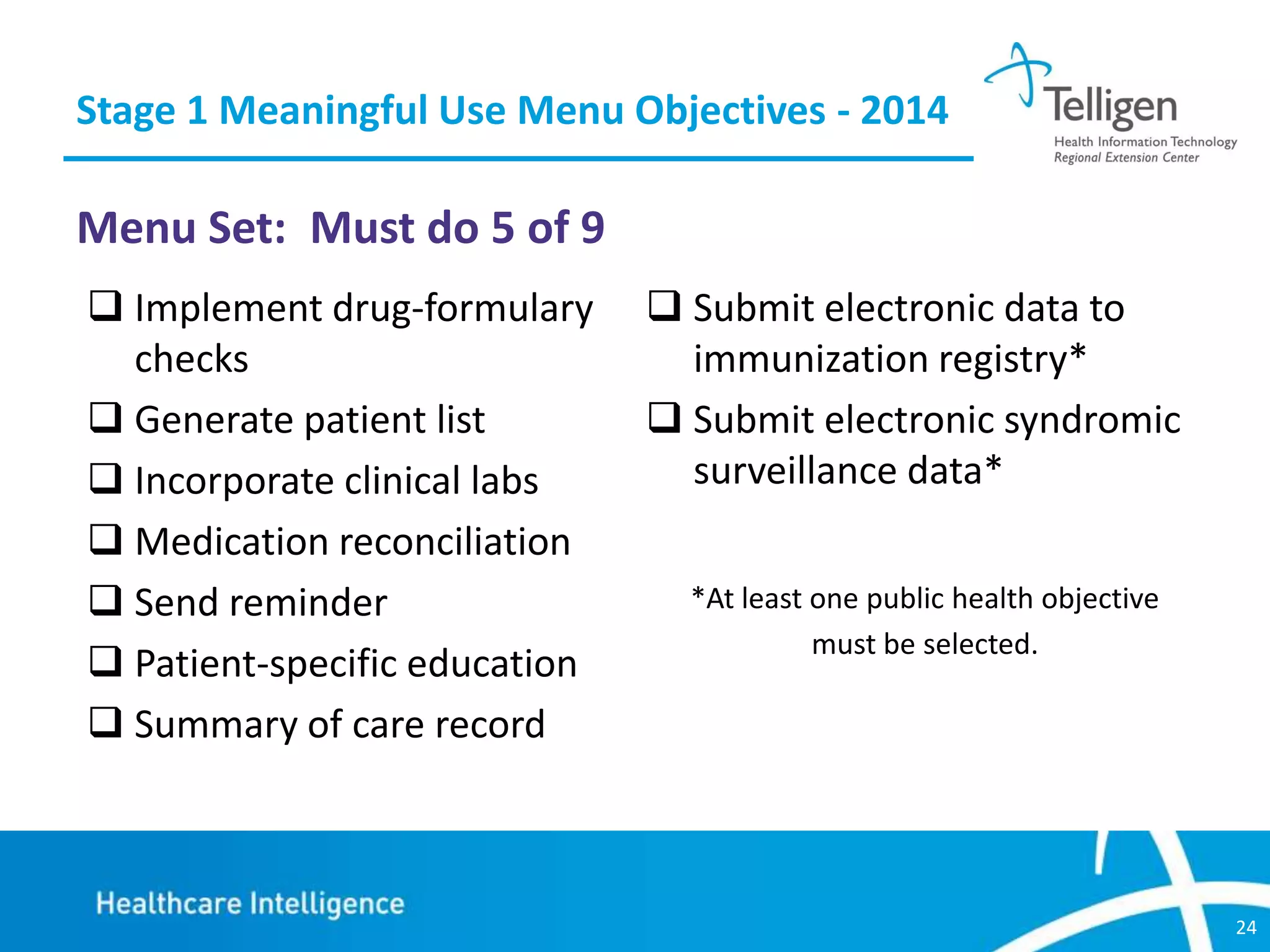
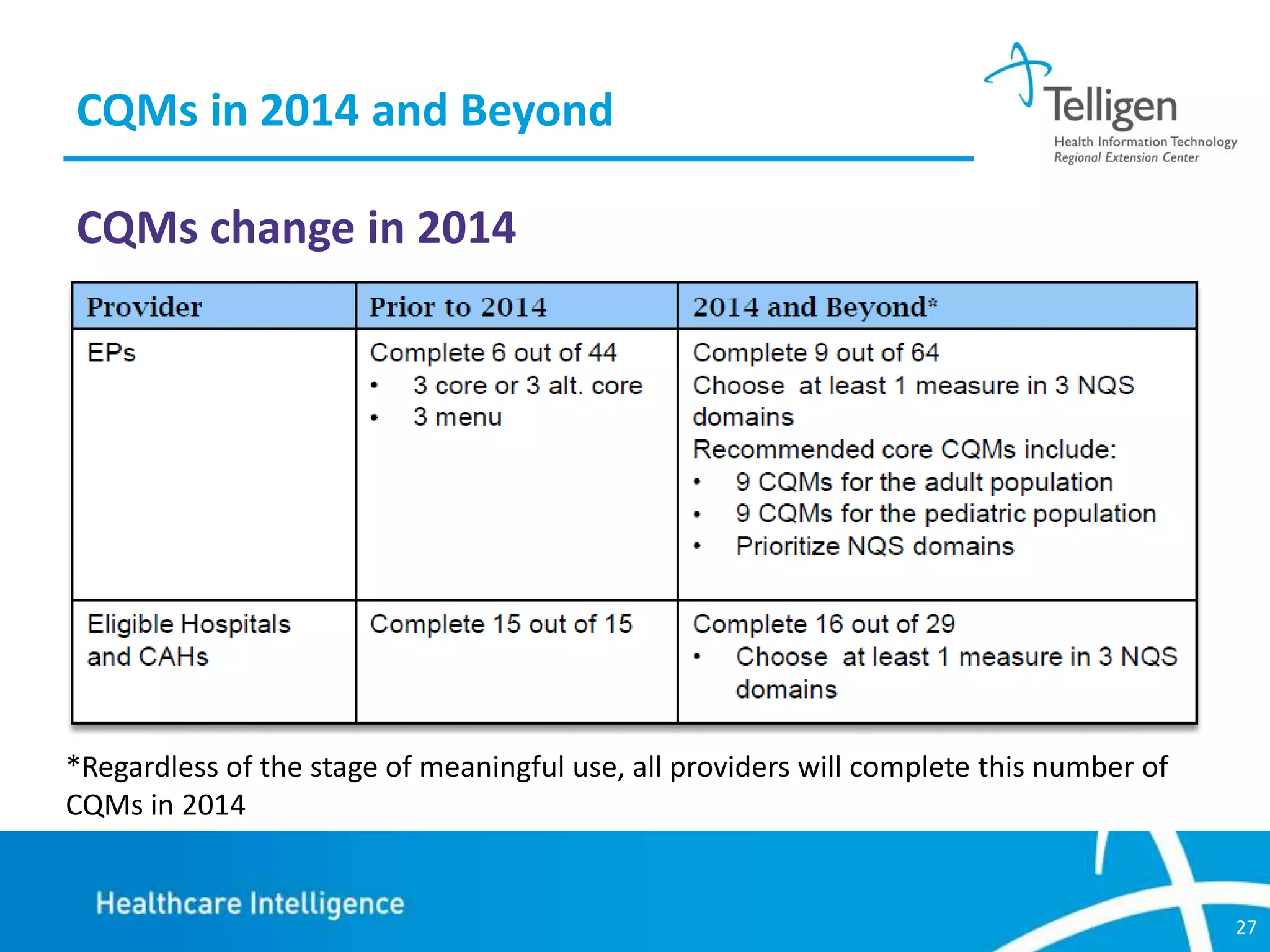
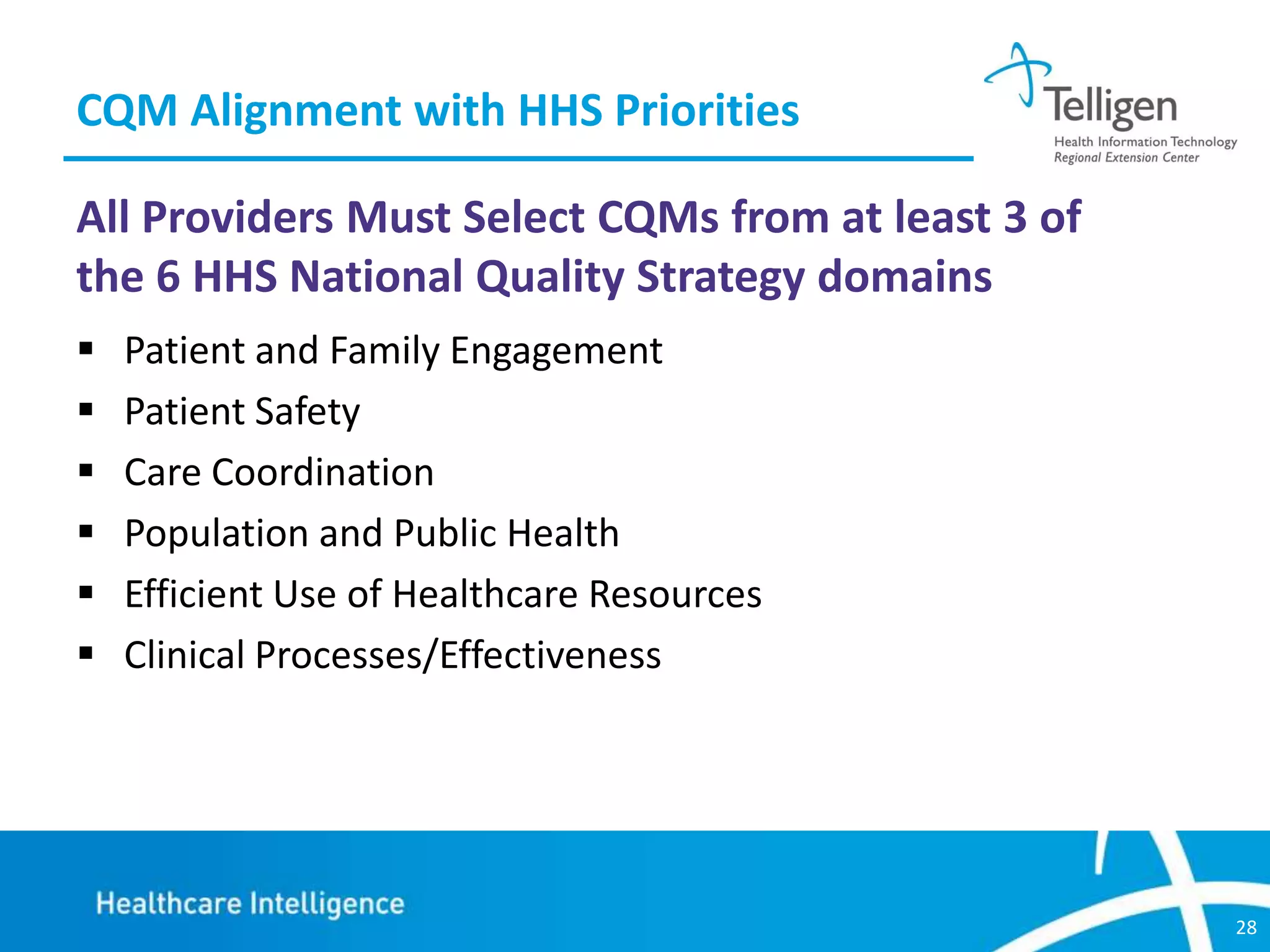
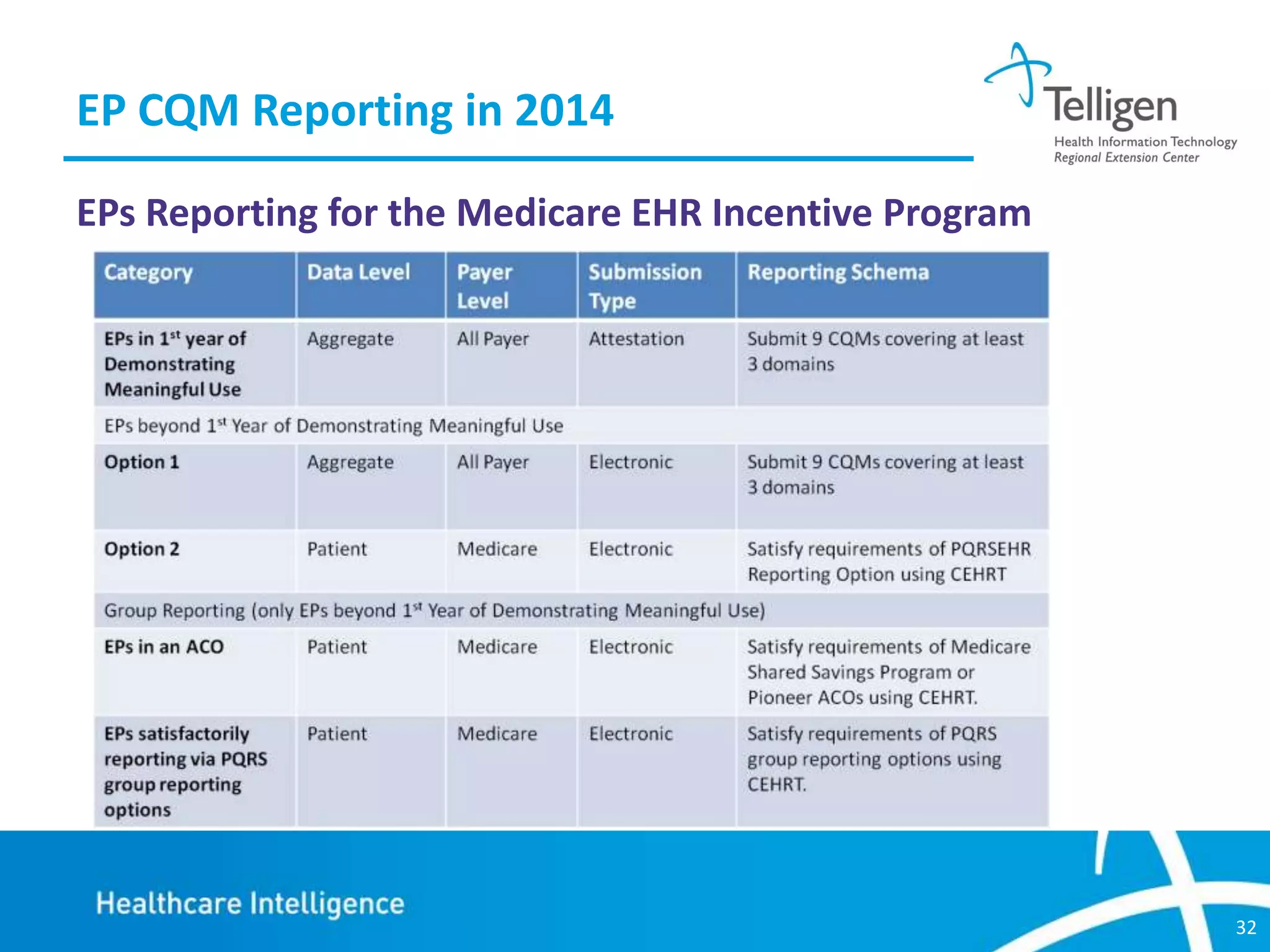
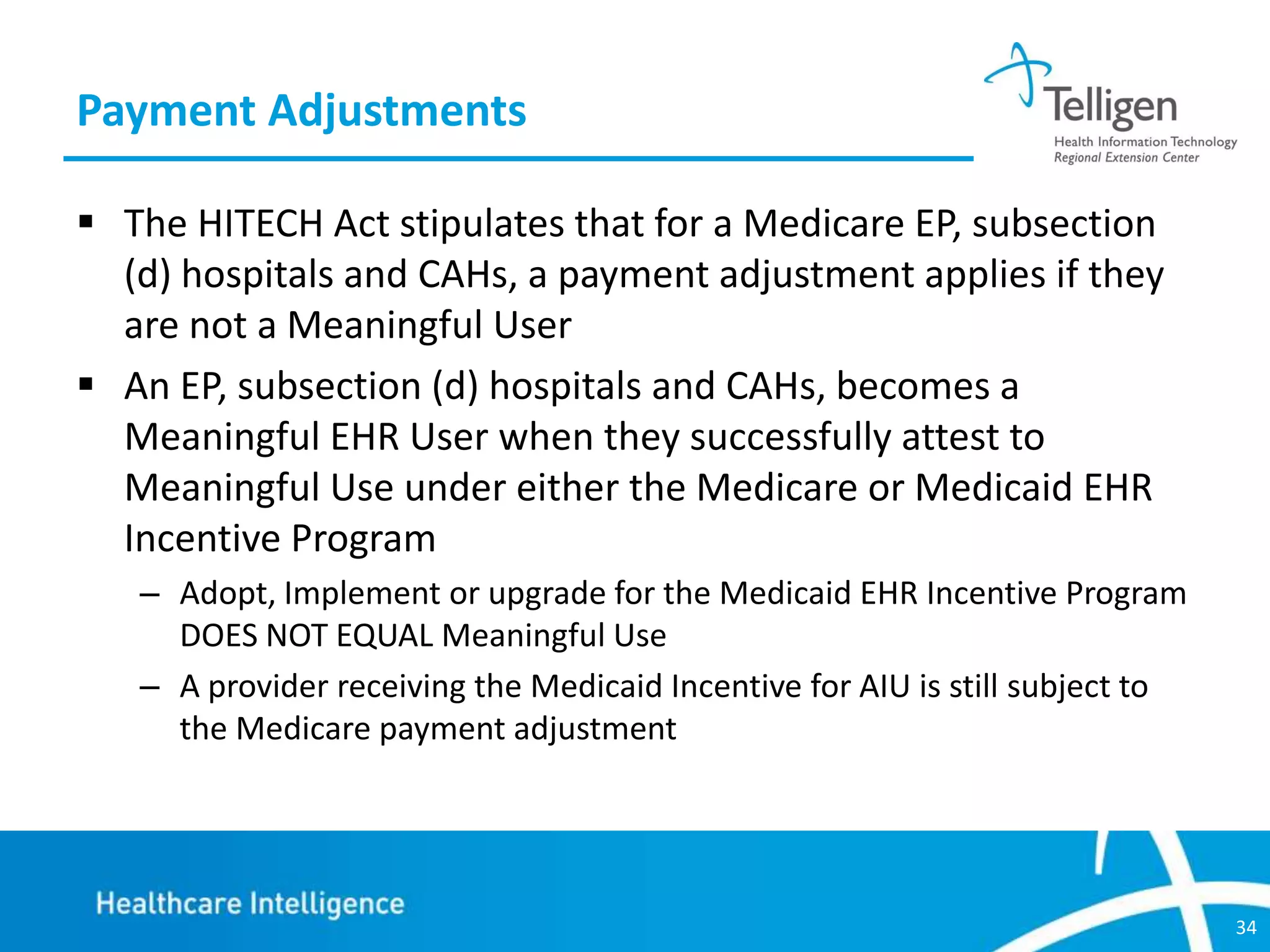
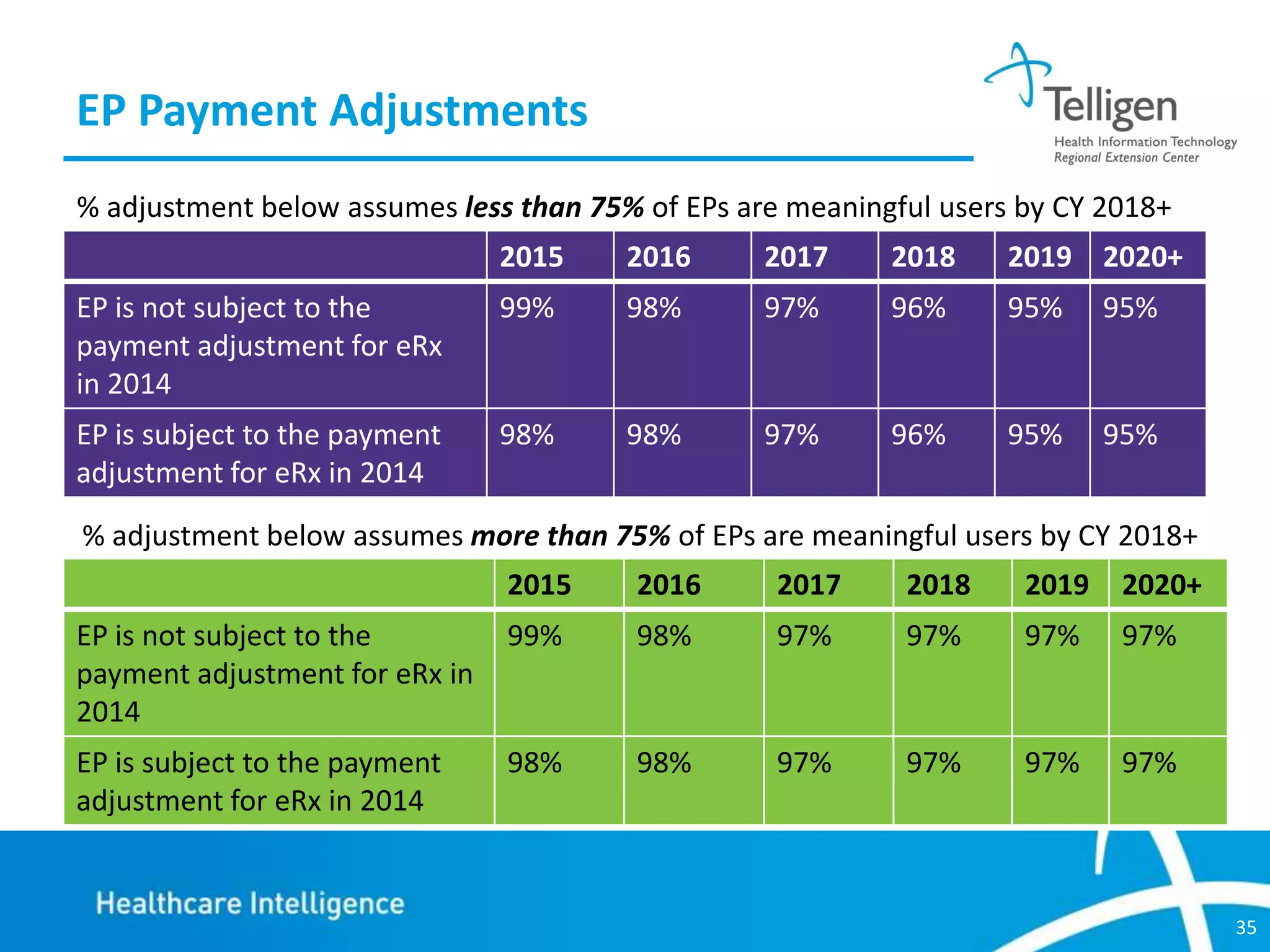
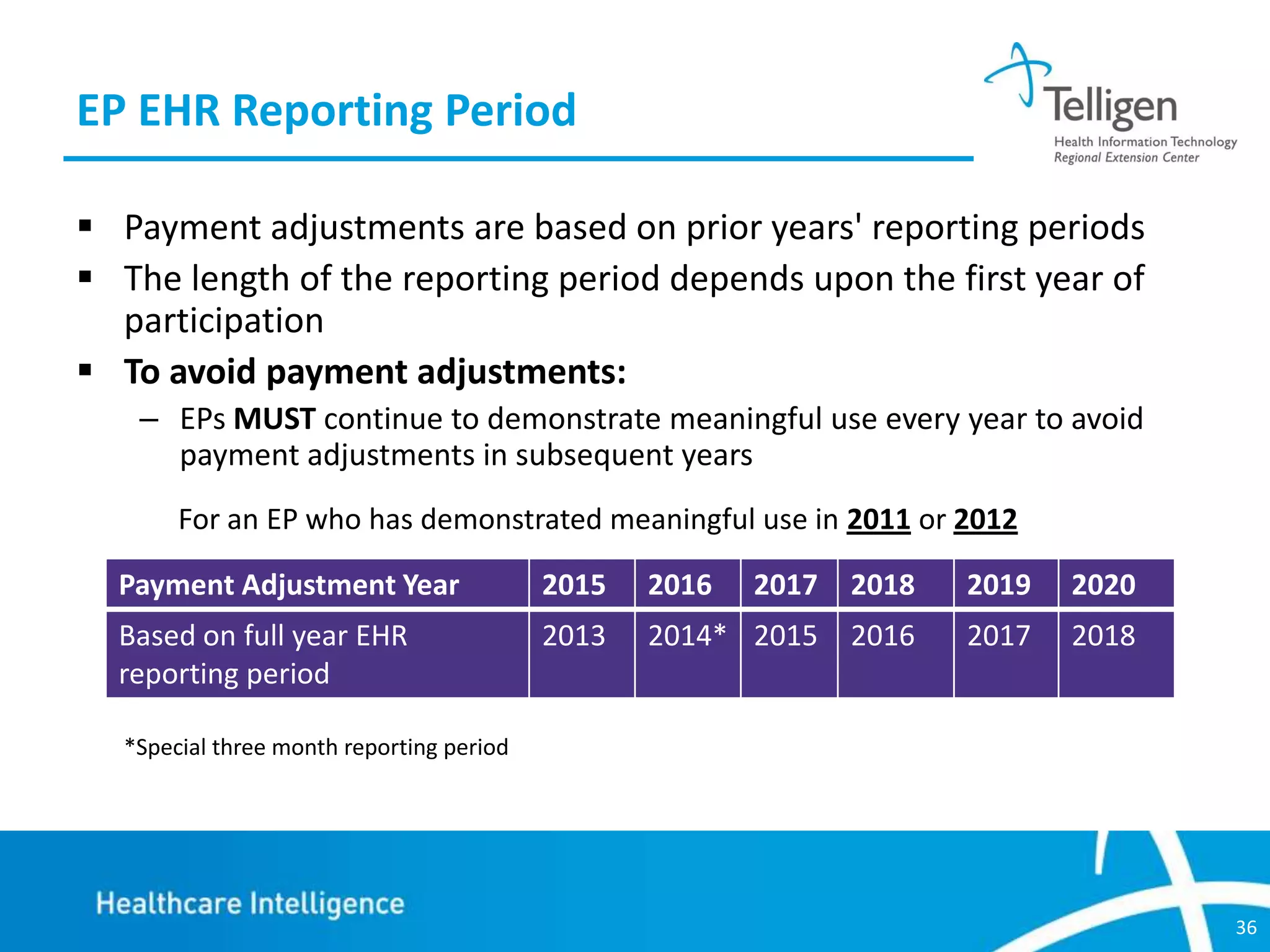
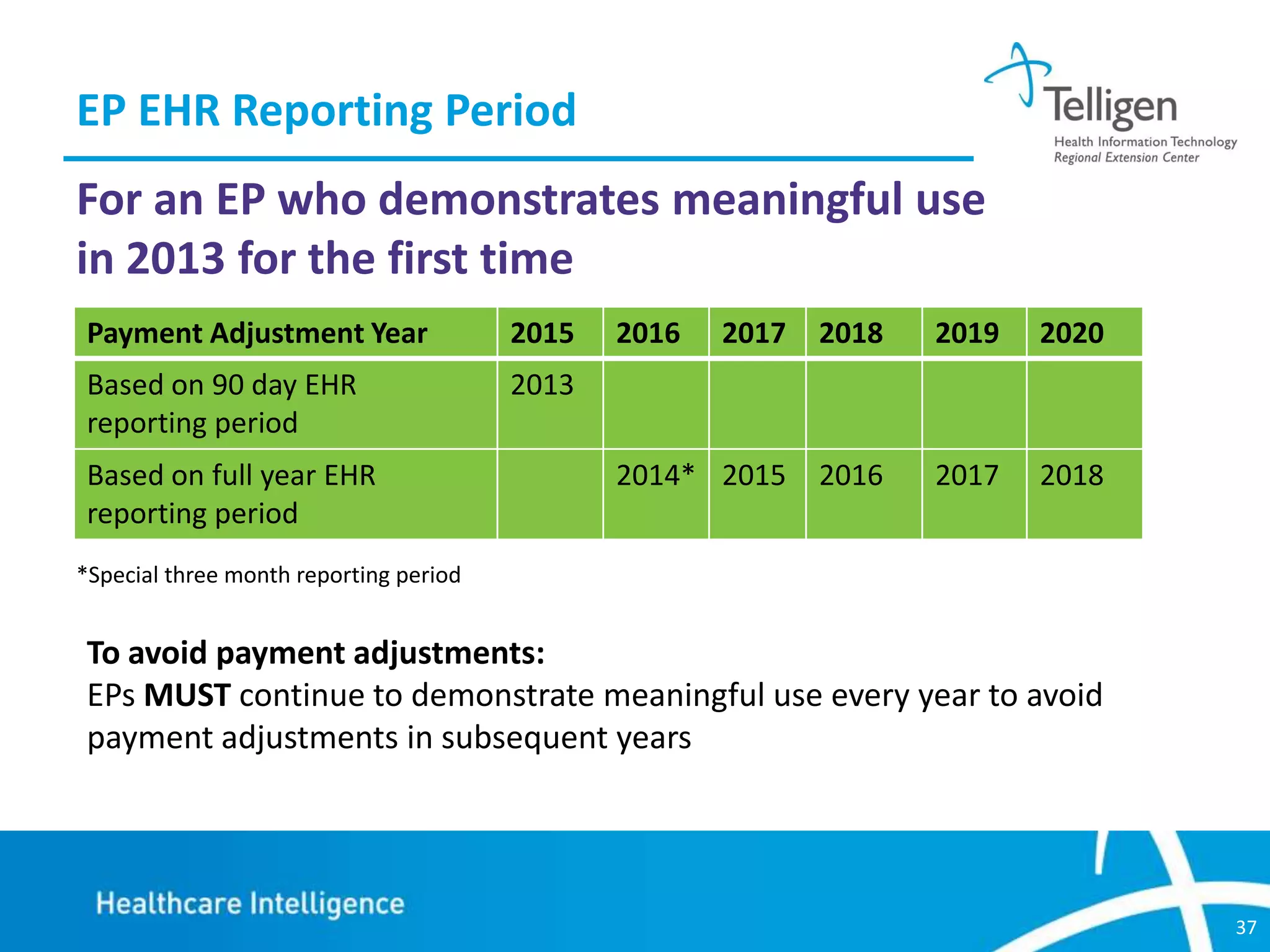
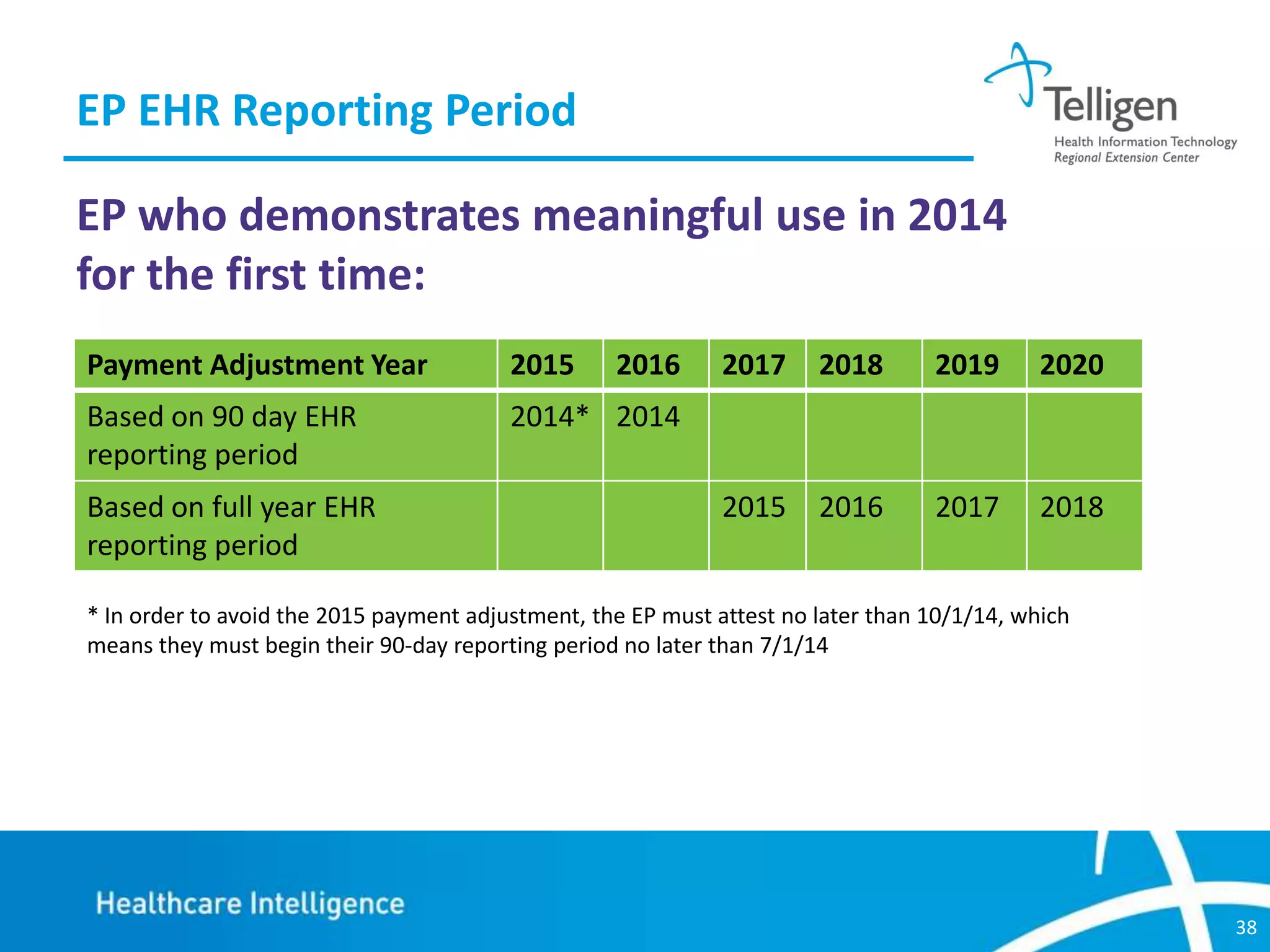
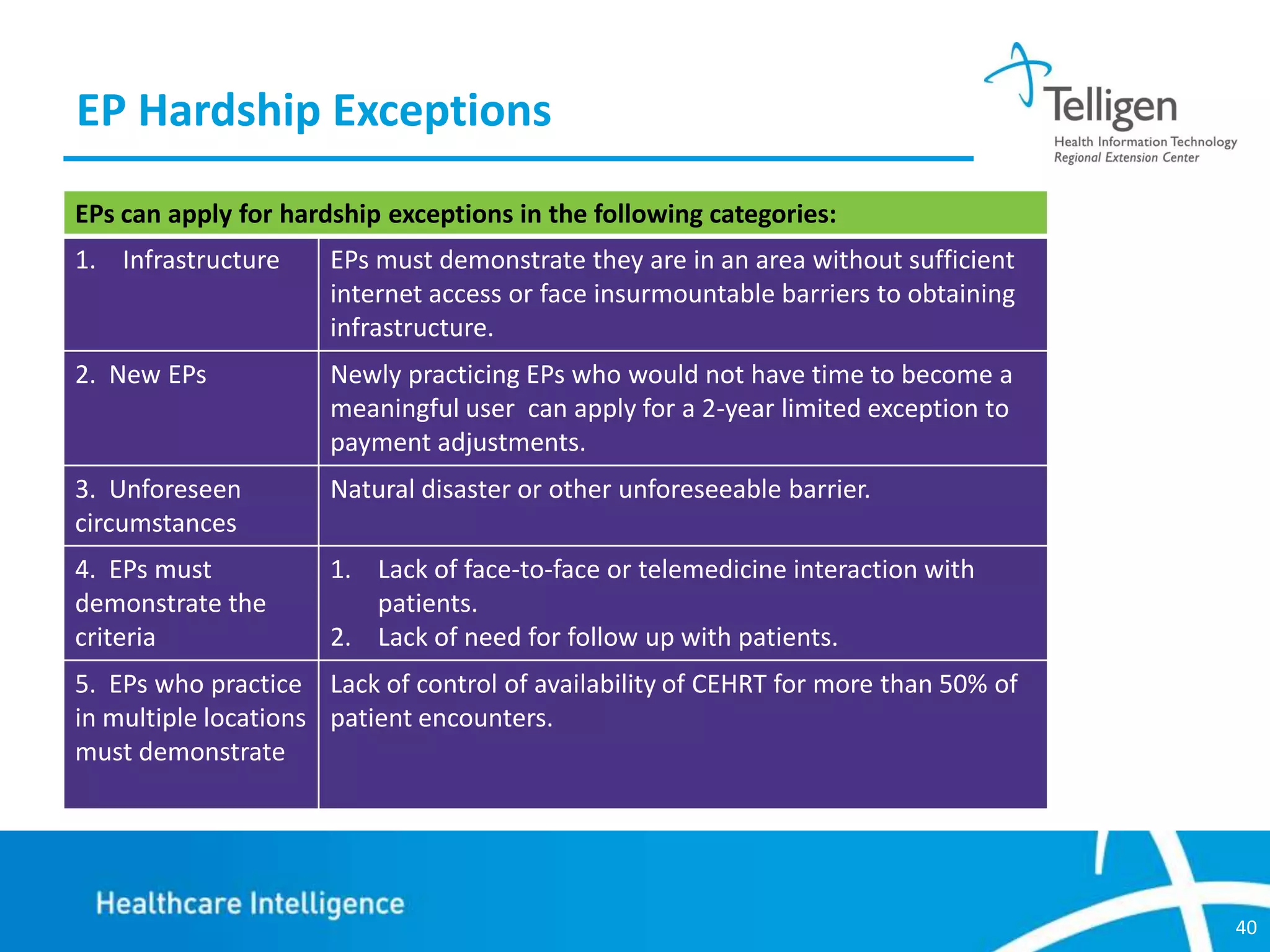
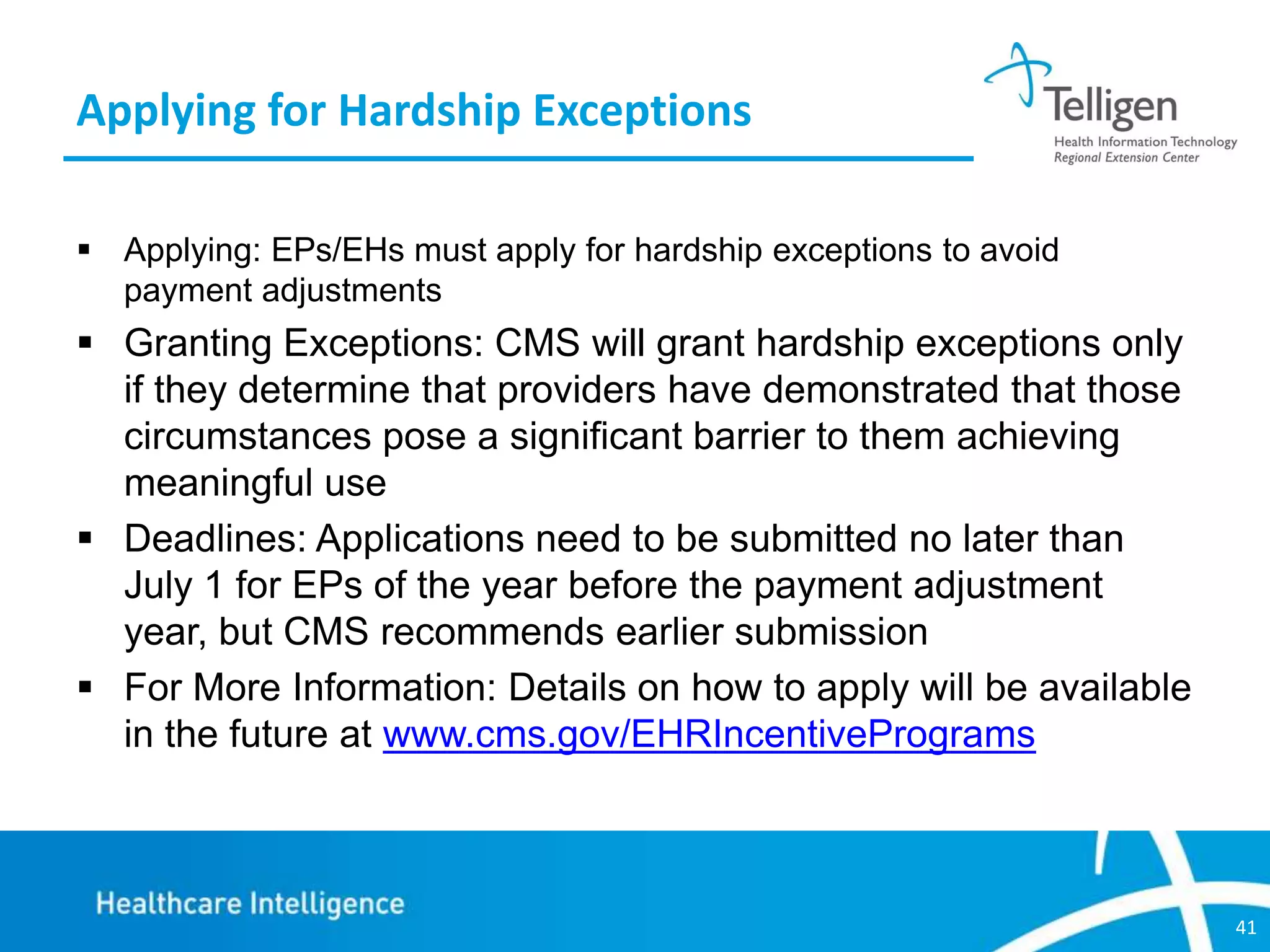
This document discusses changes to Meaningful Use Stage 1 requirements for eligible professionals in 2014. Key changes include reducing the EHR reporting period to 3 months, removing one core objective, modifying measures for CPOE and vital signs, and providing more flexibility for public health objectives and clinical quality measures. Eligible professionals must also upgrade to 2014 certified EHR technology and may be subject to Medicare payment adjustments if Meaningful Use requirements are not met.