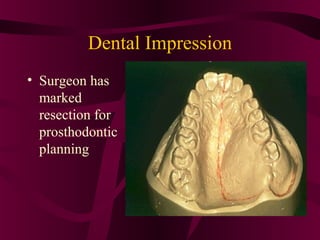
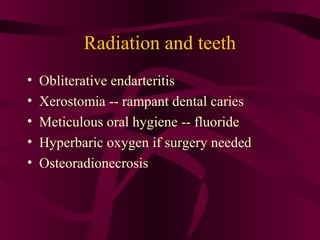
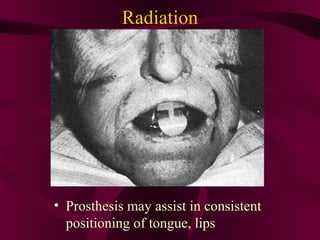
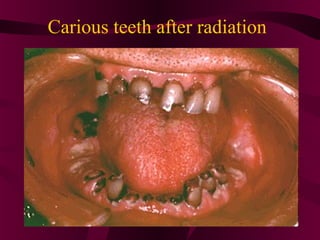
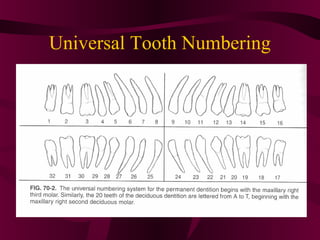
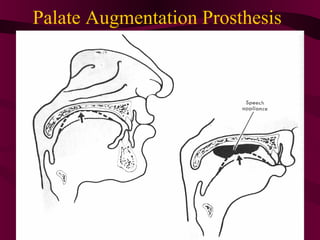
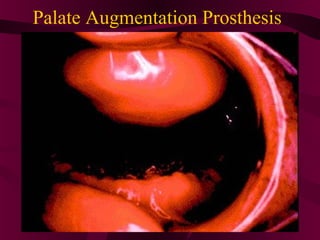
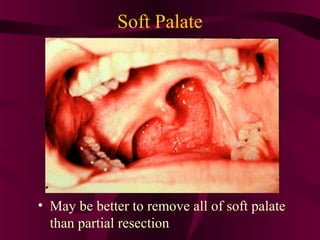
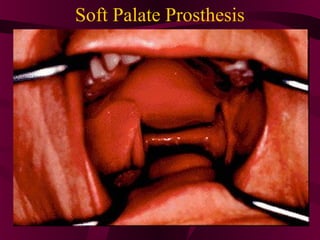
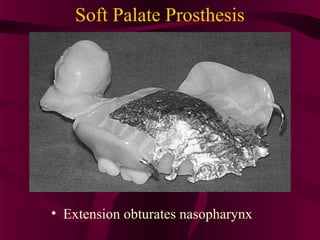
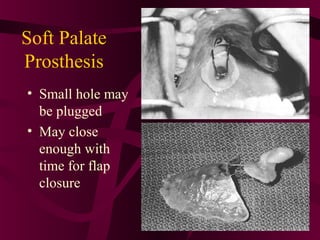
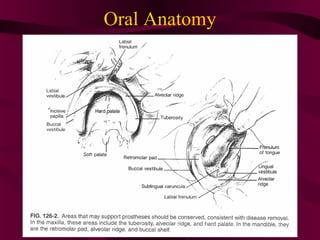
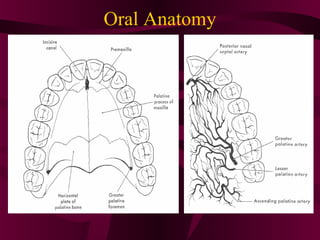
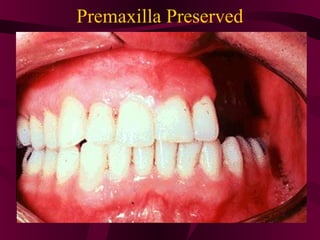
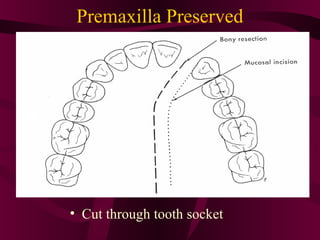
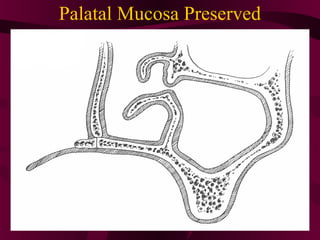
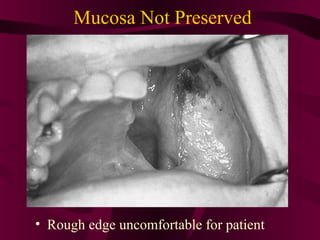
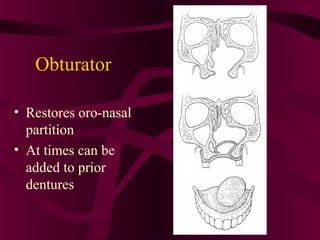
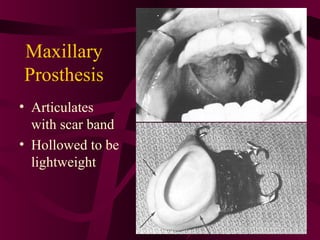
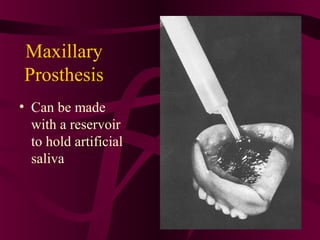
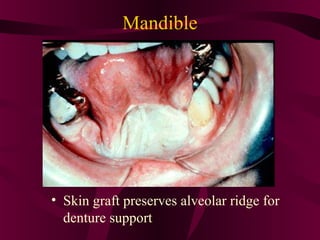
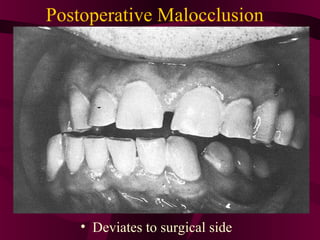
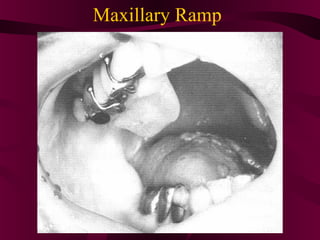
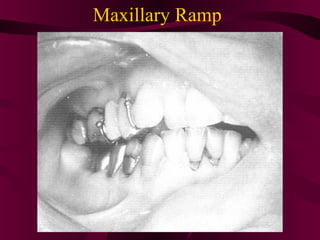
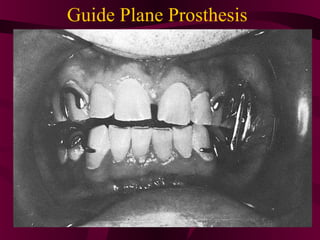
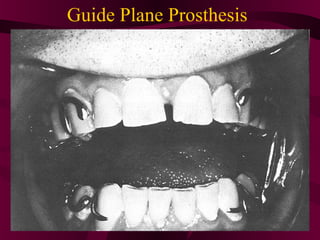
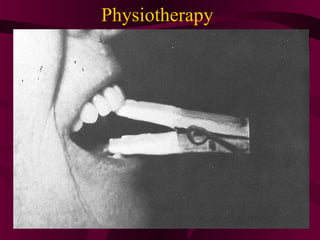
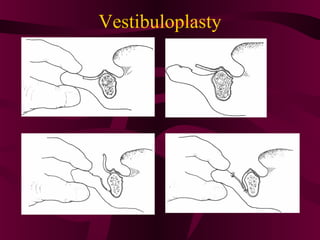
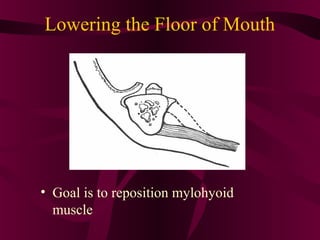
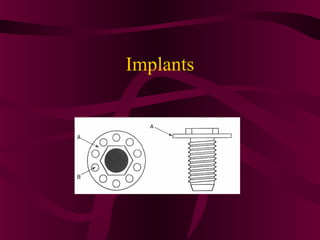
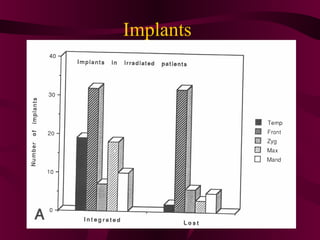
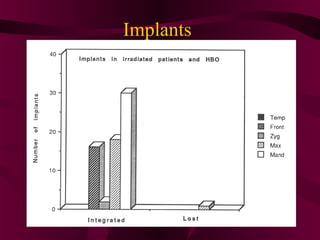
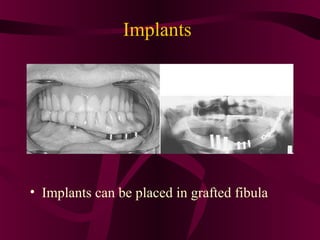
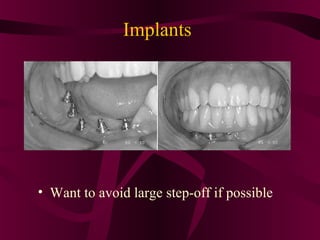
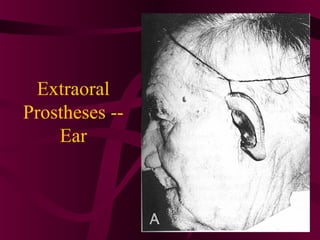
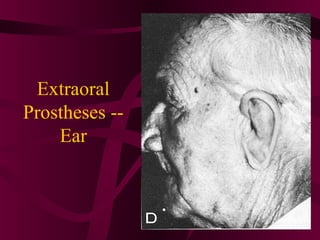
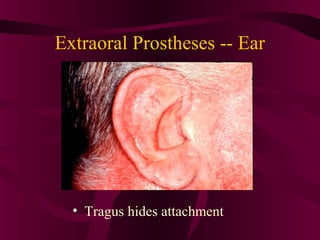
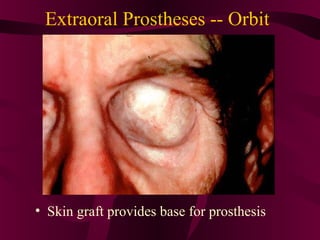
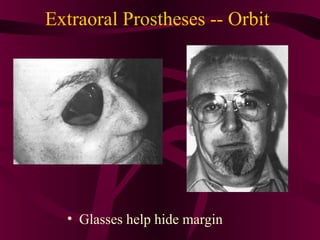
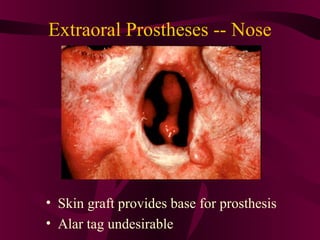
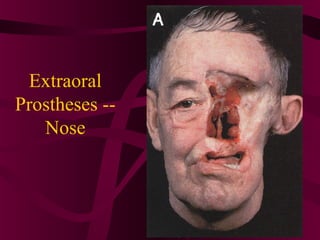
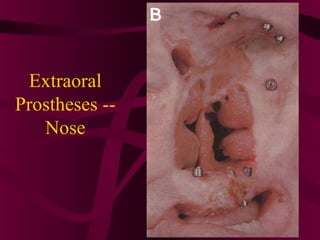
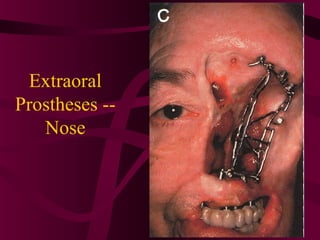
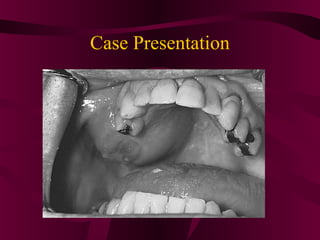
The document discusses surgical and prosthetic techniques for maxillofacial rehabilitation following cancer resection, noting that the goal is to restore both function and cosmesis through a combination of surgery, such as skin grafting, and prosthetics like obturators and implants to replace missing structures of the face, jaw, and oral cavity.