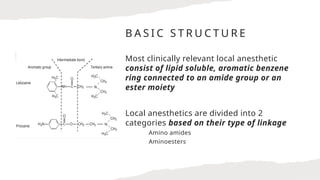
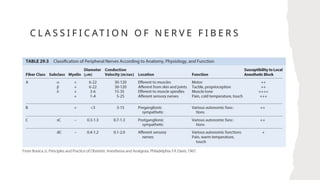
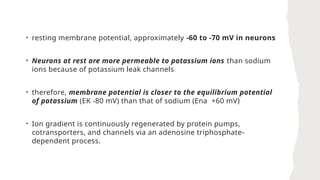
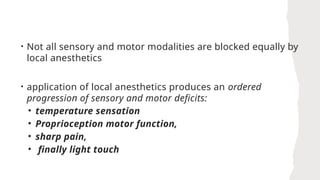
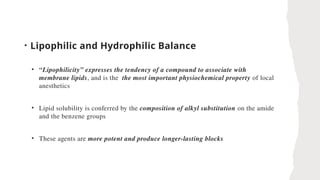
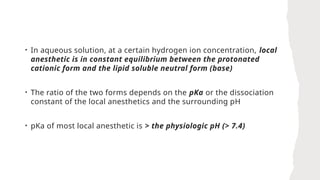
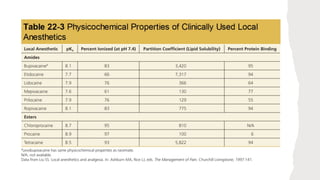
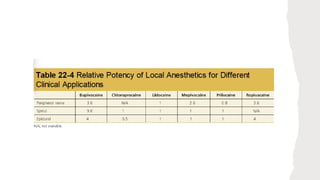
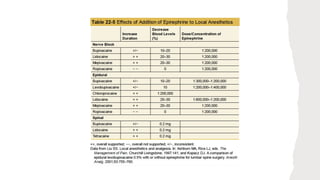
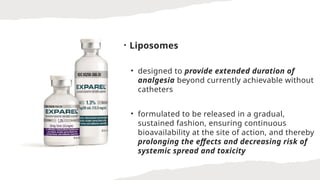
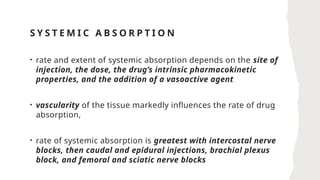
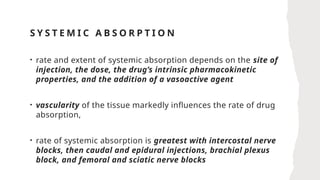
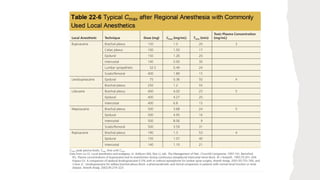
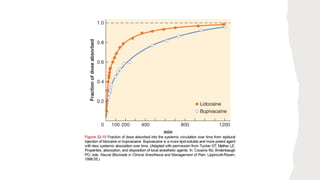
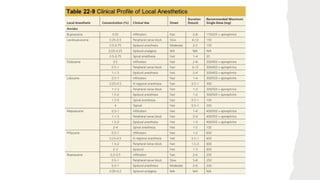
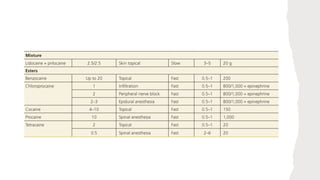
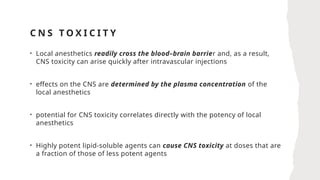
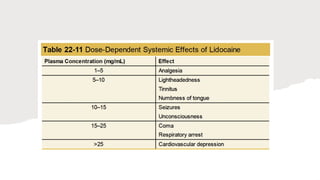
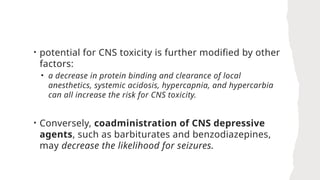
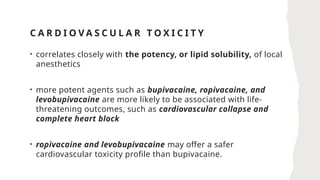
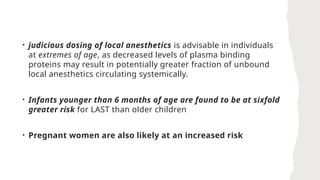
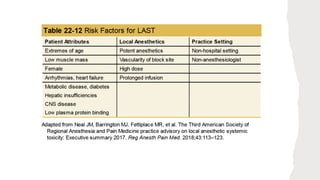
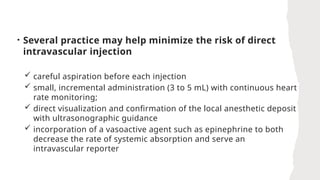
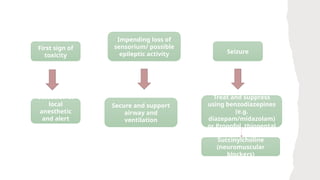
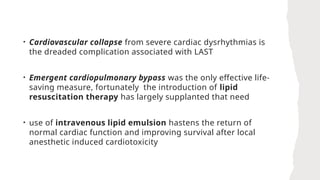
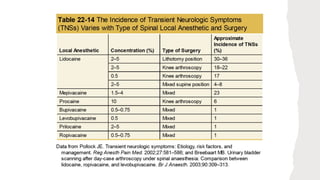
The document provides a comprehensive overview of local anesthetics, covering their pharmacology, mechanisms of action, clinical applications, and potential adverse effects. It details the structure, pharmacokinetics, and pharmacodynamics of local anesthetics while discussing systemic toxicity and its impact on the CNS and cardiovascular system. Recent advancements, clinical uses, and strategies for enhancing the efficacy and safety of local anesthetics are also presented.