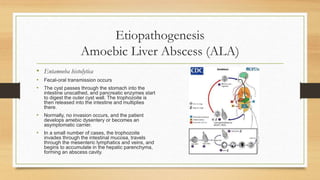
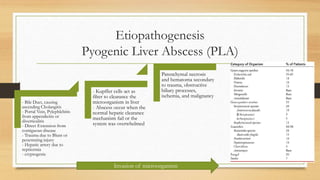
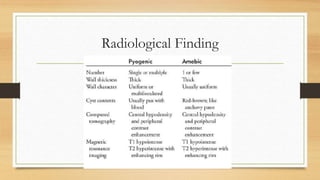
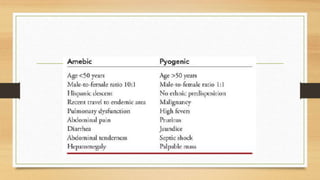
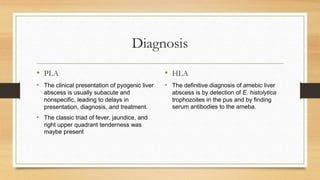
Hepatic abscesses, categorized as pyogenic (PLA) and amoebic (ALA), are encapsulated collections of pus within the liver, commonly caused by infections. The incidence of PLA is increasing due to advancements in cancer management and imaging, while ALA affects 500 million carriers worldwide. Diagnosis involves identifying E. histolytica in ALA and utilizing imaging for PLA, with treatment options including drainage and systemic medications, alongside considerations for specific patient conditions.